Table of Contents
Imagine settling into bed, only to find that shallow breathing during sleep transforms what should be a rejuvenating experience into a source of concern. For many, the phenomenon of shallow breathing when sleeping isn’t just a quirky sleeping habit; it’s a puzzle piece in the larger picture of their overall health.
But how do you distinguish between harmless heavy breathing at night and a signal that your body is trying to alert you to something more? This guide dives into the world of shallow breathing—exploring dyspnea and apnea, uncovering their distinctions, impacts, and what you can do to breathe easier and sleep better. Stay with us as we navigate the nuances of nighttime breathing, offering insights and hope for those seeking a deeper, more peaceful sleep.
What is shallow breathing while sleeping?
Imagine your breath as the ocean’s tide: it should flow in and out, deep and rhythmic, sustaining you without a second thought. However, for some, this tide ebbs too lightly during sleep, barely whispering against the shore. This is shallow breathing, a reduced breath depth that differs significantly from the full, healthy patterns we need for restorative rest.
But why does this matter? Shallow breathing at night can sneakily undermine your health, leaving the door ajar for a cascade of concerns.
Without the deep, restful breathing your body craves you might not get enough oxygen or effectively expel carbon dioxide. This imbalance can disrupt the quality of your sleep, impacting your well-being far beyond just feeling tired.
If left unaddressed, it could pave the way for more serious conditions, including cardiovascular issues or chronic fatigue, making it not just a matter of a good night’s sleep but of overall health (1).
How do I tell if I have shallow breathing during sleep?
Identifying shallow breathing can be easy to overlook. Here are some signs that can help you or your partner spot it:
Noisy sleep: Snoring, snorting, or gasping can be the body’s way of sounding the alarm. If your sleep is noisy, it might be due to obstructed airways, which can lead to or indicate shallow breathing. The louder and more persistent the noise, the more urgent it is to take notice.
Restlessness: Have you ever found your bed looking like a battleground in the morning? Tossing and turning might be your body’s struggle for more air. Disorganized bedding can be a silent witness to the night’s efforts to breathe deeply.
Chronic fatigue: Waking up feeling like you’ve run a marathon, not rested, points to unrefreshing sleep. Daytime drowsiness and a feeling of fatigue that coffee can’t cure suggest that your sleep quality is compromised, potentially by shallow breathing.
To truly know, consider monitoring your sleep, either through a sleep study or with the help of wearable technology. Being mindful of these symptoms and acknowledging them is the first step toward better health.
Dyspnea vs apnea: Understanding the distinctions
When it comes to sleep-related breathing issues, two terms often emerge: dyspnea and apnea.
While both can disrupt a night’s rest and impact overall health, they are distinct conditions with their own set of implications.
Dyspnea
Dyspnea is essentially a subjective feeling of difficulty breathing. Linked mainly to heart and lung issues, it can also arise from anemia, anxiety, or obesity.
Some types, like paroxysmal nocturnal dyspnea, cause individuals to wake up gasping for air while sighing dyspnea involves frequent sighing to ease ongoing breathlessness.
Apnea
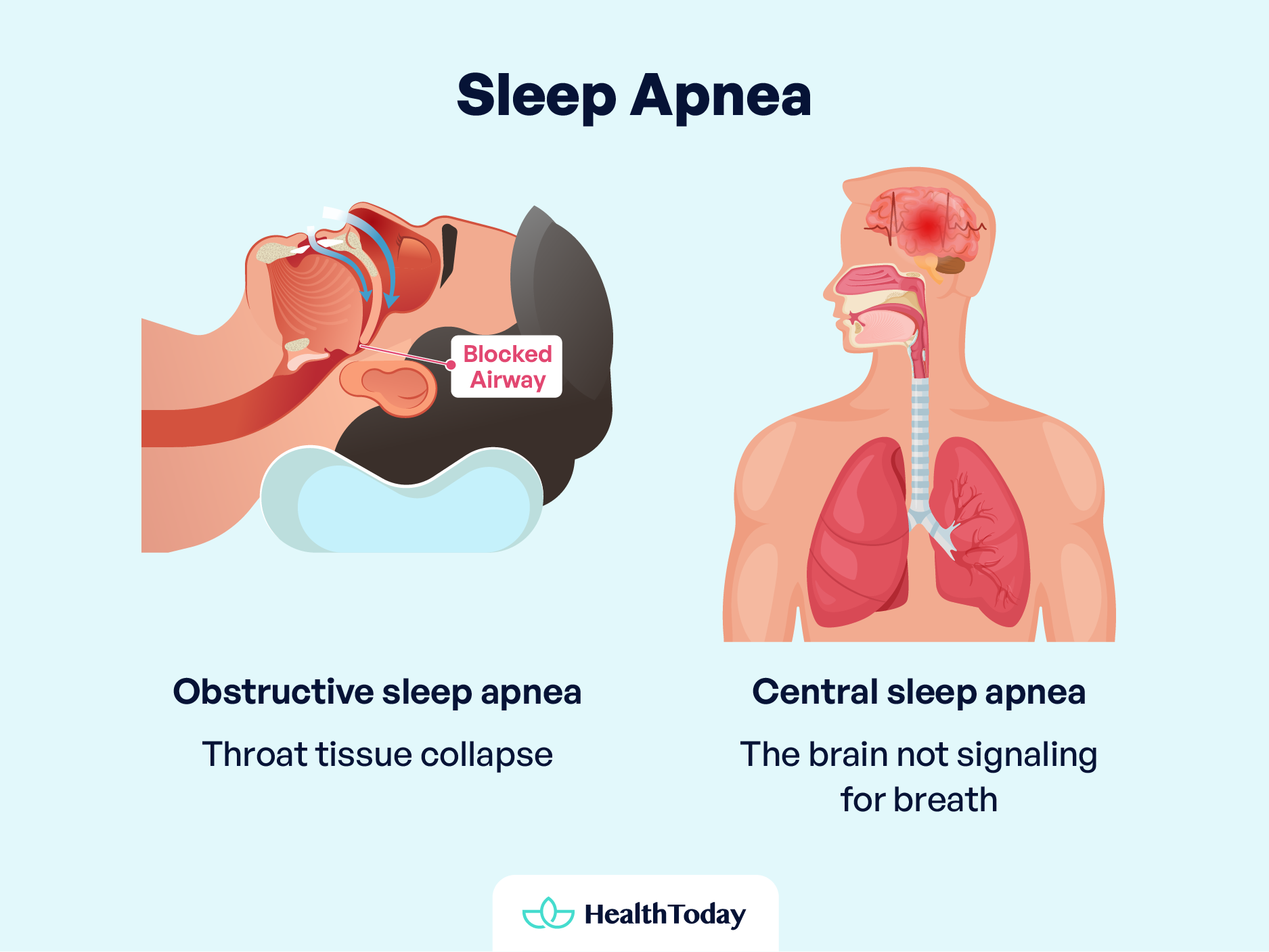
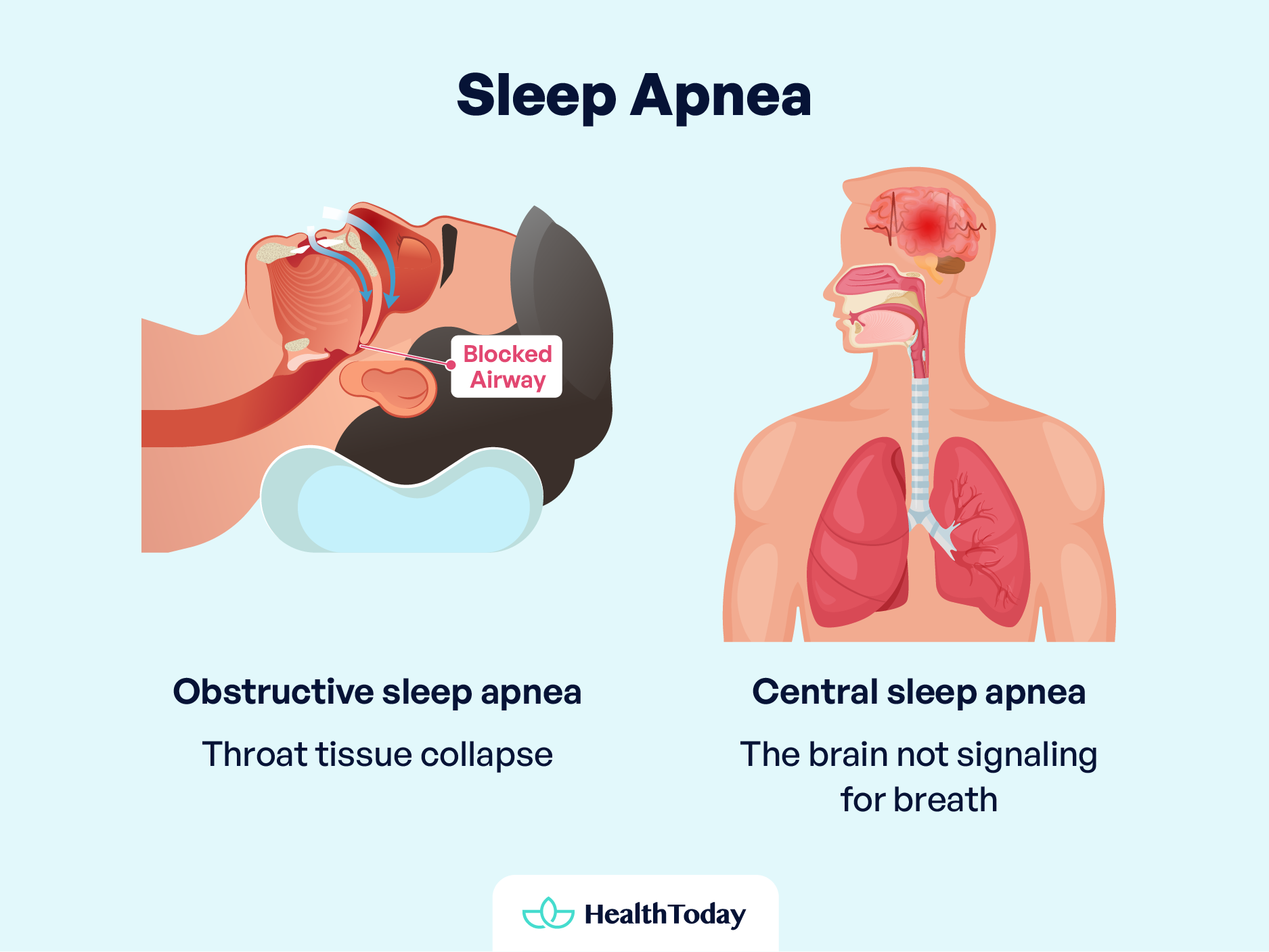
Apnea involves breathing interruptions or shallowness caused by airway blockage or neural signal issues.
Obstructive sleep apnea, the most common type, results from throat tissue collapse, leading to gasping or snorting. Central sleep apnea is due to the brain not signaling for breath and is linked to neuromuscular or heart conditions (2).
Symptoms: A comparative look
Symptoms of dyspnea (3):
For dyspnea, monitoring involves being attuned to feelings of breathlessness, particularly if these sensations wake you from sleep or if you frequently sigh.
- Sensations of air hunger or chest tightness.
- The feeling that one must exert extra effort to breathe.
- Rapid breathing or rapid heart rate.
- Wheezing or stridor, indicating noisy breathing.
Symptoms of sleep apnea (4):
Signs of apnea often require an outside observer, like a partner might notice episodes of snoring or breathing cessation. Restlessness, daytime fatigue, and the physical act of gasping or choking upon waking are critical indicators.
- Noisy sleep, including snoring, snorting, or gasping, pointing to obstructed airways.
- Restlessness and disturbed bedding hint at the body’s struggle for oxygen.
- Chronic fatigue, resulting from unrefreshing sleep and leading to daytime drowsiness and a weakened immune response.
- Specific types of people, including gender, post-menopausal women, and individuals with overweight/obesity, may have a heightened risk profile for obstructive sleep apnea (OSA).
Both conditions can cause similar issues like tiredness and trouble sleeping. However, they have different causes and symptoms.
Dyspnea involves feeling out of breath and struggling to breathe deeply, while sleep apnea is marked by breaks in breathing and the body’s struggle to breathe well at night.
Dyspnea vs. apnea: How it may affect the body
Knowing how dyspnea and apnea can affect your health over time is crucial. If ignored, both can seriously harm your health in different ways. Understanding their impacts helps you take early action to manage and treat these conditions.
The long-term effects of apnea
Sleep apnea poses several risks if untreated. The intermittent oxygen deprivation and sleep disruption associated with apnea can have profound effects on the body:
- Cardiovascular stress: Sudden drops in blood oxygen levels increase blood pressure and strain the cardiovascular system (4). This strain can elevate the risk of heart attacks, strokes, and abnormal heart rhythms.
- Metabolic syndrome: Sleep apnea is linked with metabolic syndrome, a cluster of conditions including high blood pressure, abnormal cholesterol levels, high blood sugar, and increased waist circumference (5).
- Type 2 diabetes: The condition also heightens the risk for insulin resistance, making individuals more susceptible to type 2 diabetes (6).
- Liver complications: People with sleep apnea are more likely to have abnormal liver function tests and signs of liver scarring (7).
Moreover, sleep apnea can complicate the use of medications and recovery from surgery, as those affected may have more pronounced breathing difficulties, especially when sedated or lying on their back.
The long-term effects of dyspnea
While dyspnea—or shortness of breath—may not always signal a severe condition, it can be a symptom of underlying health issues that, if severe and left untreated, may lead to life-threatening situations.
Immediate medical attention is necessary if dyspnea is accompanied by symptoms such as sudden difficulty breathing, chest pain, fast or irregular heartbeat, high fever, or blue discoloration of the skin (cyanosis).
Chronic dyspnea can significantly affect quality of life and may indicate serious conditions such as:
- Heart diseases: Severe dyspnea could point to heart problems, including heart failure or coronary artery disease, where the heart struggles to supply the body with enough blood and oxygen.
- Lung conditions: Persistent shortness of breath may indicate chronic obstructive pulmonary disease (COPD) or pulmonary hypertension, severely limiting lung function and oxygen uptake (8).
- Severe anemia: A condition characterized by a lack of red blood cells to carry adequate oxygen to the body’s tissues, making it hard to breathe (9).
Can sleep apnea / dyspnea go away? Treatment insights
Facing difficulties like dyspnea or sleep apnea, learning about treatments can give hope. Remember that getting better breathing and sleep involves unique plans based on expert advice and custom treatments.
Treatment options for sleep apnea
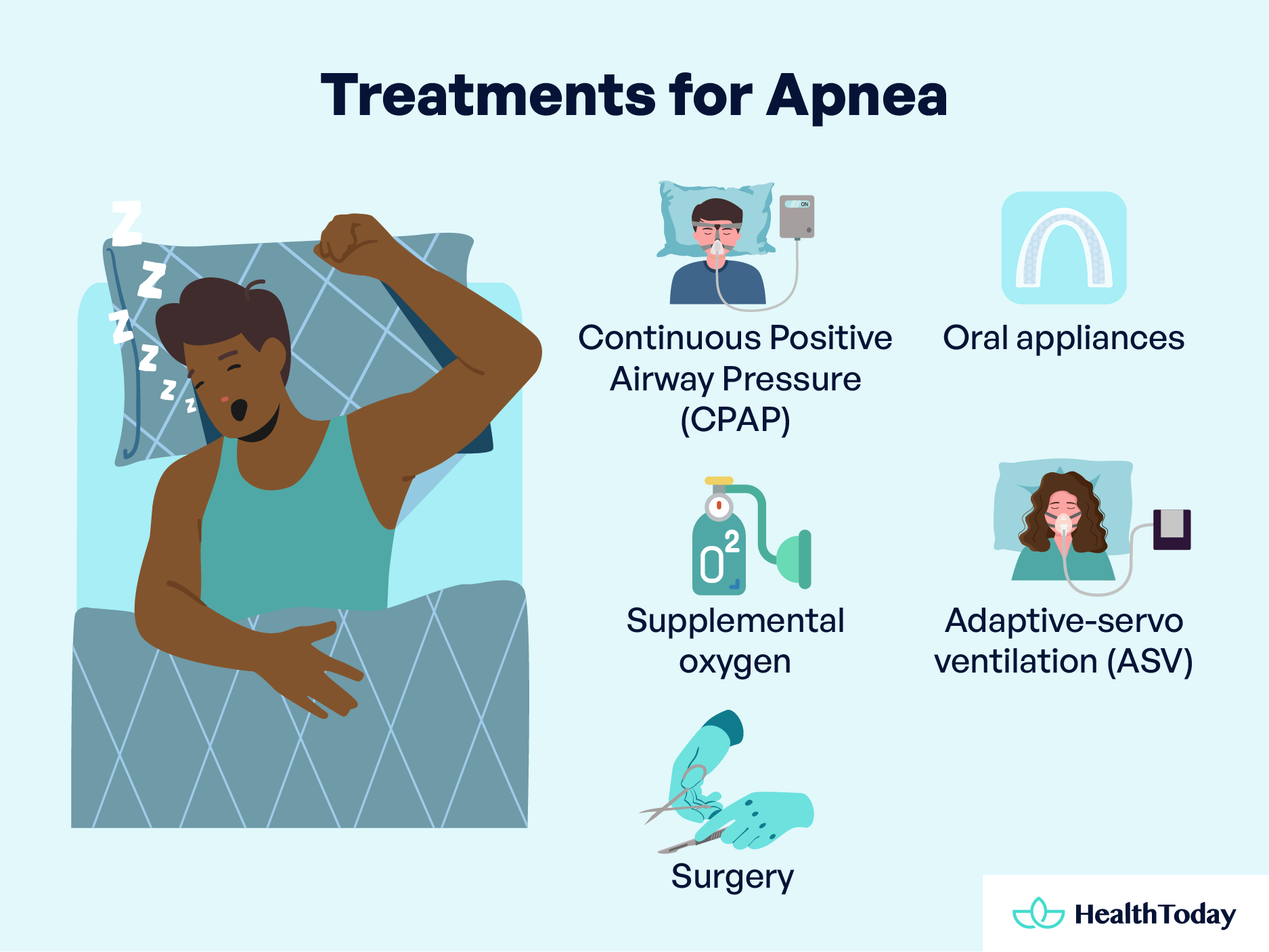
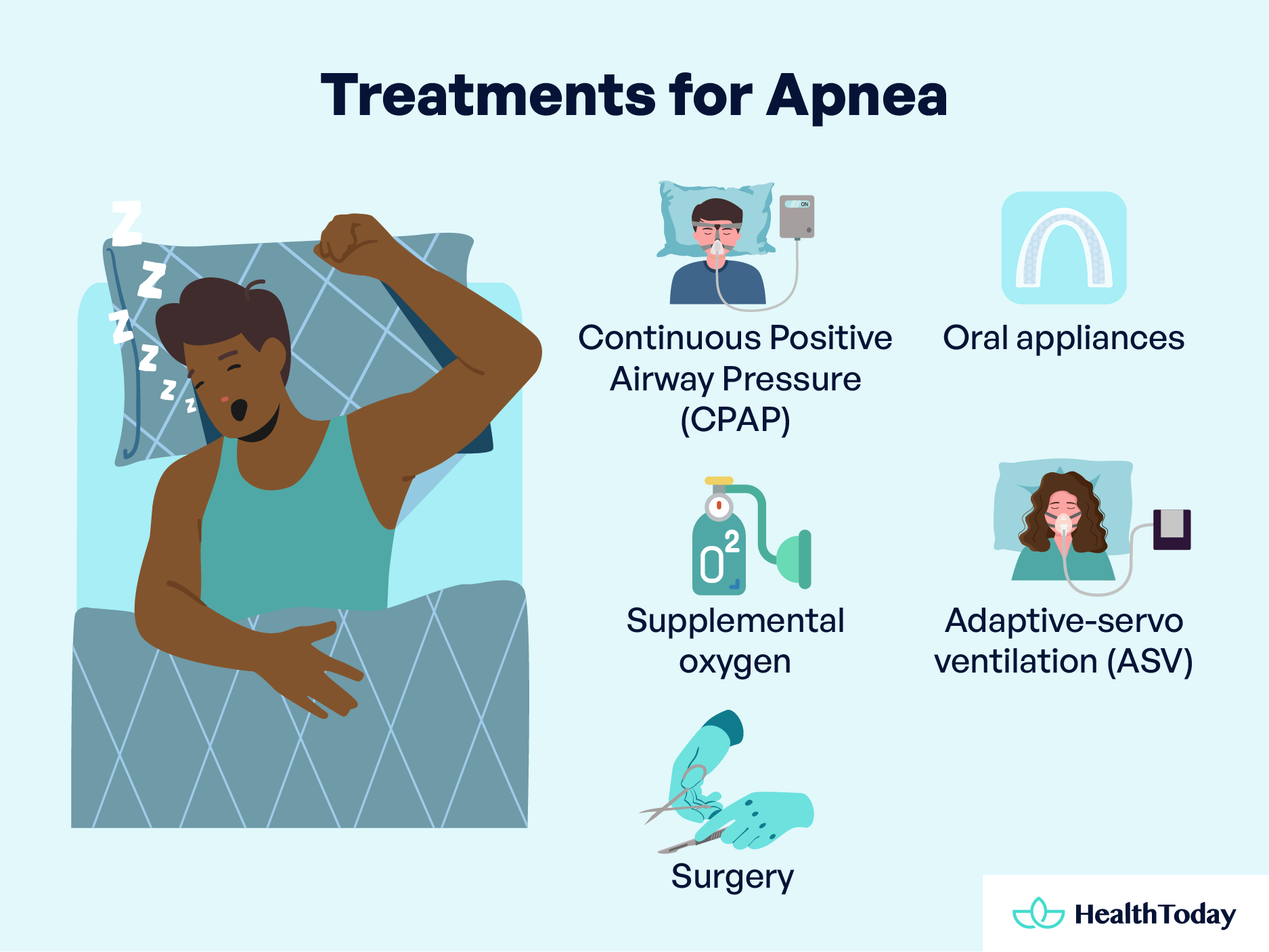
The management of sleep apnea depends on the severity of the condition. For those with mild cases, lifestyle adjustments such as weight loss, quitting smoking, or addressing nasal allergies may significantly alleviate symptoms. However, more pronounced cases necessitate a diverse array of treatments:
- Continuous Positive Airway Pressure (CPAP): A cornerstone treatment that uses air pressure through a mask to keep airway passages open, combating apnea and snoring (10). For those finding CPAP masks uncomfortable, alternative designs and adjustments can enhance comfort and compliance.
- Oral appliances: These devices can help keep the throat open and are particularly useful for those who find CPAP challenging. Collaborate with a dentist to find the most suitable option for you.
- Supplemental Oxygen: Used in cases of central sleep apnea, different forms of oxygen delivery can help maintain proper oxygen levels during sleep.
- Adaptive Servo-Ventilation (ASV): An advanced treatment that adapts to your breathing pattern, ASV effectively manages complex sleep apnea by normalizing breathing patterns (11).
- Surgery: In some cases where conventional treatments haven’t provided relief, surgical options such as tissue removal, jaw repositioning, or nerve stimulation may be considered.
Treatment options for dyspnea


The approach to treating dyspnea focuses on the underlying cause. Whether the breathlessness stems from a chronic condition or acute anxiety, tailored treatments can offer significant relief:
- Exercise: Strengthening the heart and lungs reduces their workload, improving breathing efficiency.
- Relaxation and breathing exercises: These techniques can ease the sensation of breathlessness, which is especially beneficial for dyspnea related to anxiety.
- Medication: Bronchodilators can relax airways in conditions like asthma and COPD, while other medications may target pain or anxiety contributing to dyspnea (12).
- Oxygen therapy: Prescribed for low blood oxygen levels, oxygen therapy can be delivered via masks or nasal tubes, providing crucial support for more efficient breathing (13).
Other causes of shallow breathing while sleeping


While conditions like sleep apnea are commonly associated with disruptions in standard breathing patterns during sleep, other factors may contribute to shallow breathing, often unnoticed but equally significant.
Heart Failure
Heart failure, a condition where the heart doesn’t pump blood as well as it should, can lead to fluid buildup in the lungs (14). This accumulation can cause difficulty breathing, especially when lying down, as it interferes with the lungs’ ability to expand fully, leading to shallow breathing during sleep.
The body’s attempt to compensate for the reduced oxygen circulation can exacerbate this condition, making it a critical factor to consider.
Asthma and other lung disorders
Conditions like asthma or chronic obstructive pulmonary disease (COPD) can significantly affect breathing patterns, not only during the day but also at night. These disorders cause the airways to narrow or become blocked, leading to reduced airflow and, consequently, shallow breathing (15).
Nighttime symptoms may be particularly pronounced for some individuals, disrupting sleep and reducing oxygen levels in the blood.
Allergies
Allergic reactions, especially those involving the respiratory system, can also lead to shallow breathing while sleeping.
Allergens like dust, pet dander, or pollen can trigger inflammation in the airways, causing congestion and reduced air movement. This response, while protective, can compromise breathing depth and quality during sleep.
Obesity
Obesity significantly impacts respiratory function due to the excess weight on the chest and abdomen, restricting lung expansion and leading to shallow, less effective breaths. Furthermore, obesity is a known risk factor for obstructive sleep apnea, compounding the challenges faced by those struggling with weight issues (16).
Genetic factors
In some cases, genetic predispositions can influence the development of conditions that affect breathing, including structural abnormalities in the airway or lung function. While not everyone with a genetic predisposition will experience shallow breathing during sleep, it is a factor worth considering, especially in the presence of family history.
Drug use or overdose
Substances that depress the central nervous system, including certain medications, alcohol, and recreational drugs, can significantly slow respiratory rate and depth. This effect can be particularly dangerous during sleep when the body’s natural mechanisms to compensate for respiratory distress are less active (17).
Pneumonia and heartburn
Unexpected conditions like pneumonia, an infection that inflames the air sacs in one or both lungs and heartburn—a symptom of acid reflux, can also contribute to shallow breathing (18, 19). While their primary symptoms may differ, both can affect nighttime breathing comfort and efficiency.
What you can do to reduce shallow breathing during sleep
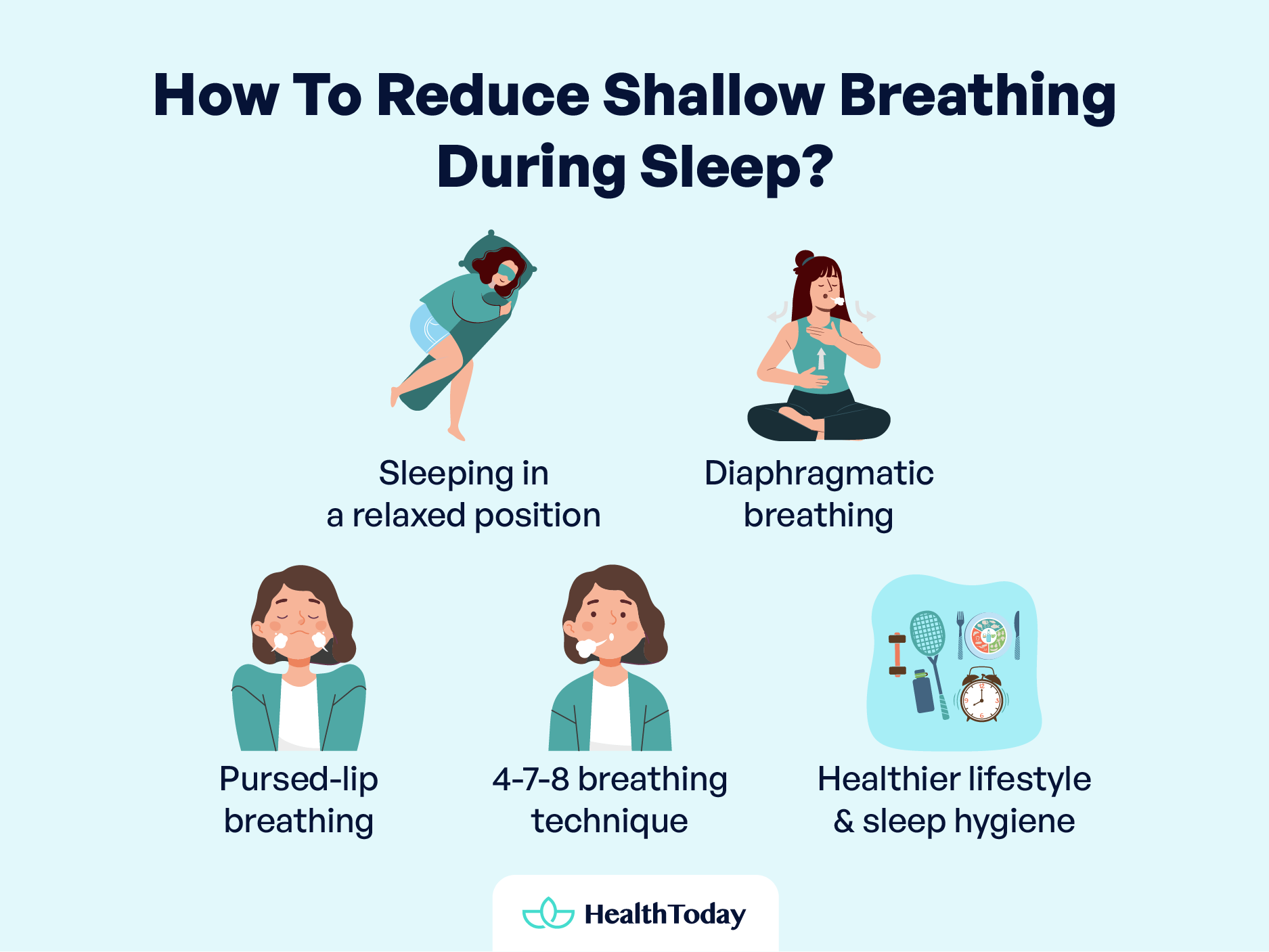
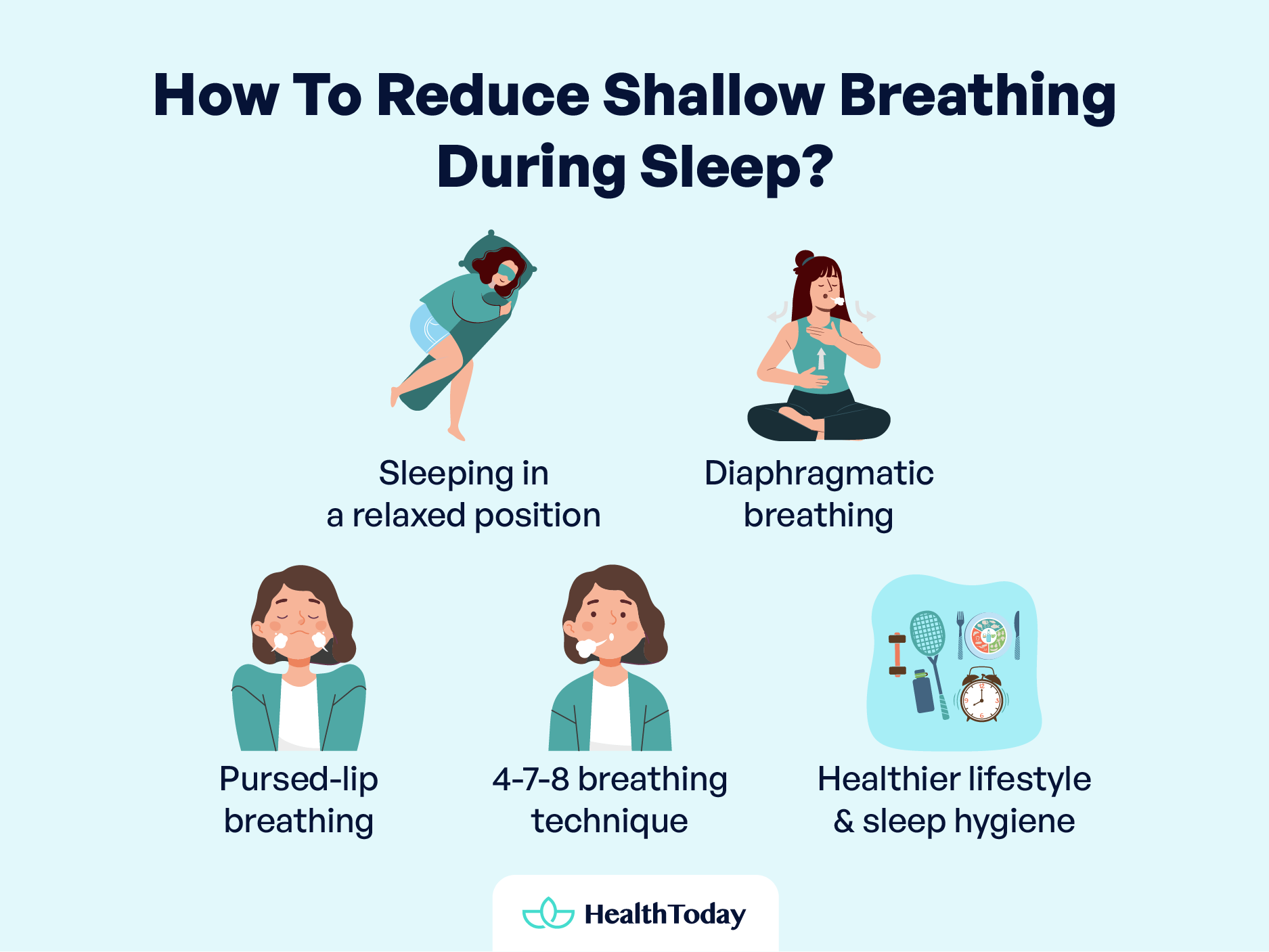
For those nights when sleep seems elusive due to shallow breathing, there are practical steps you can take to find relief and embrace a night of deeper, more restful sleep. By incorporating some simple strategies into your nightly routine, you can improve your breathing and enhance your overall sleep quality. Let’s explore some tips that are both hopeful and grounded in care.
Sleeping in a relaxed position
Finding the proper sleep position is crucial for facilitating easier breathing.
For many, sleeping on the side with a pillow between the legs and head elevated helps open the airways.
Alternatively, lying on your back with your head elevated and knees bent, supported by a pillow under your knees, can also promote better breathing. Experiment to find which position feels most natural and improves your breathing.
Diaphragmatic breathing
Diaphragmatic breathing, or abdominal breathing, focuses on engaging the diaphragm for deeper, more efficient breaths (20). Here’s a simple way to practice:
- Lie down with your legs slightly apart and relax your body.
- Place one hand on your stomach and the other on your chest to monitor your breathing.
- Breathe deeply through your nose, ensuring your abdomen rises more than your chest.
- Exhale slowly through your mouth, focusing on emptying your lungs fully.
Regular practice, even for just 5 to 10 minutes a day, can significantly improve your breathing depth and efficiency, especially during sleep.
Pursed-lip breathing
This technique is particularly beneficial for those experiencing shortness of breath (21). Pursed-lip breathing helps control the pace of your breathing, making each breath more effective:
- Inhale slowly through the nose for two counts.
- Exhale gently through pursed lips for four counts.
This method not only slows down breathing but also helps increase lung efficiency.
4-7-8 Breathing technique
Developed by Dr. Andrew Weil, the 4-7-8 breathing technique is a powerful method for signaling to your body that it’s time to sleep. It involves a specific pattern that helps slow down your breathing:
- Exhale completely through your mouth, making a whoosh sound.
- Close your mouth and inhale quietly through your nose to a count of four.
- Hold your breath for seven seconds.
- Exhale completely through your mouth, making a whoosh sound to a count of eight.
- This is one breath. Now, inhale again and repeat the cycle three more times for a total of four breaths.
Practicing this technique before bed can help relax your mind and body, preparing you for a restful night’s sleep.
Embracing a holistic approach
While these breathing exercises and sleep positions can significantly reduce shallow breathing, it’s also important to consider lifestyle adjustments that support overall health. Weight management, avoiding alcohol before bedtime, and maintaining good sleep hygiene can further improve breathing issues.
Additionally, ensuring a clean and allergen-free sleeping environment can make a big difference for those with allergies.
When to see a doctor
Recognizing when to seek professional medical advice is crucial. Let’s identify the signs that signal it’s time to reach out to a healthcare provider, emphasizing the importance of taking action for your health.
Make an appointment if you (4, 3):
- Experience frequent or persistent shortness of breath.
- Find yourself waking up at night due to difficulty breathing.
- Notice wheezing or a whistling sound when you breathe or feel tightness in your throat.
Additionally, pay attention to symptoms that accompany shortness of breath, such as:
- Swollen feet and ankles.
- Trouble breathing when lying flat.
- Fever accompanied by chills and cough.
- An increase in the severity of breathlessness over time.
Consulting a healthcare provider allows for a comprehensive evaluation of your symptoms. Through diagnostic tests and assessments, they can identify any underlying issues contributing to your breathing difficulties.
Treatment might include medication, lifestyle adjustments, or specific therapies aimed at addressing the root cause of your symptoms. Remember, early intervention can significantly improve your quality of life and prevent potential complications.
Can children have shallow breathing while they sleep?
Much like adults, children can experience variations in their breathing patterns due to common culprits like respiratory infections, asthma, or even sleep apnea. Keep an ear out for snoring or pauses in breath—these are tell-tale signs that your little one might be having a bit more than a bad dream.
How many breaths per minute is normal sleeping?
A healthy adult at rest typically takes about 12 to 20 breaths per minute. When you’re asleep, this number can dip slightly lower, thanks to the relaxed state of your body and decreased metabolic demands. So, if you’re counting breaths instead of sheep, numbers slightly below 12 aren’t necessarily a cause for alarm.
What is the life expectancy of someone with sleep apnea?
Untreated sleep apnea can potentially cause heart disease, high blood pressure, and diabetes, which can all lower your lifespan. However, with treatment, the prognosis brightens considerably. Getting that sleep apnea under control can mean you’re back in the running for a normal life expectancy.
Can dyspnea be mental?
Yes, dyspnea can indeed have psychological roots. Anxiety, stress, and panic disorders are known to crash the breathing party, making you feel breathless without a physical cause in sight. It’s all about how the brain interprets signals, sometimes turning the “I’m slightly anxious” into a full-blown “I can’t breathe” scenario. Mental or not, dyspnea deserves attention and a chat with a healthcare provider.
Can dyspnea last for months?
If dyspnea lasts for months, it may indicate serious health problems like asthma, COPD, or heart issues. Don’t ignore long-term dyspnea; it’s your body’s way of saying you need to see a doctor to find out what’s wrong.
Summary
We’ve explored the difference between shallow breathing when sleeping, dyspnea, and apnea, and their effects on health. Identifying signs, like heavy breathing at night, is crucial.
We discussed causes from heart issues to allergies and shared techniques like the 4-7-8 breathing method to improve breathing.
Most importantly, we highlighted the need for professional advice for persistent symptoms. Remember, addressing shallow breathing during sleep is key to better health and well-being.















Comments
0