Table of Contents
Rheumatoid arthritis is a chronic autoimmune disease that affects between 0.3 percent and 1.2 percent of the world’s population, according to epidemiological data (1). It is characterized by inflammation of the joints, which causes pain, stiffness, and difficulty in movement. In addition, this disease can affect other bodily organs, such as the bones, lungs, and nerves, and can cause anemia, among other symptoms.
Although rheumatoid arthritis can occur at any age, it tends to appear more frequently between the ages of 30 and 60 (1). However, it can also affect children and older adults.
Some risk factors associated with rheumatoid arthritis are family history of the disease, gender (women are more likely to develop it than men), as well as some lifestyles (2).
Early and accurate diagnosis is essential to effectively treat rheumatoid arthritis and prevent flare-ups, which can lead to a better quality of life for those affected. Keep reading to learn more about this disease and how to deal with it effectively.
How does arthritis affect the body?
Rheumatoid arthritis (RA) is an autoimmune disease that affects more than 18 million people worldwide. About 70 percent of individuals living with rheumatoid arthritis are women, and 55 percent are older than 55 years (3).
When a person has rheumatoid arthritis, the immune system, which normally protects the body against external invaders like bacteria and viruses, becomes overactive and mistakenly attacks healthy cells of the body itself. In the case of RA, this attack primarily targets the mobile joints, causing inflammation, pain, and damage to the joint tissue.
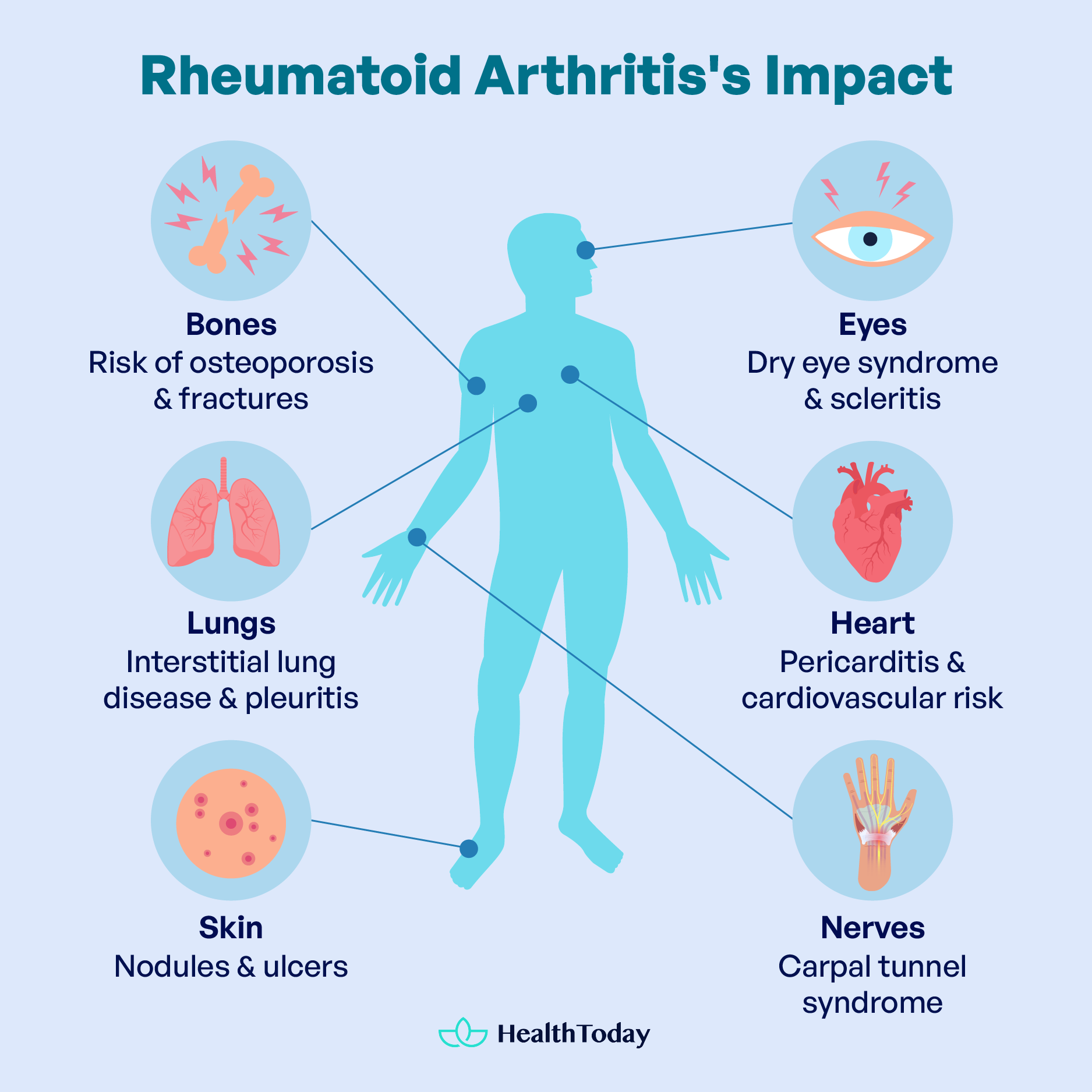
Rheumatoid arthritis is not limited to the joints alone. In some cases, it can affect other systems of the body, such as the skin, bones, eyes, lungs, heart, and nervous system.
Who does rheumatoid arthritis affect the most?
The cause of rheumatoid arthritis is unknown, but certain factors increase the risk (4):
- Individuals with a family history of autoimmune disease
- Age group between 30-60 years
- Female sex
- Smokers
- Overweight individuals
- Individuals are exposed to environmental factors such as air pollution
RA symptoms in the body
The typical clinical presentation of rheumatoid arthritis (RA) may vary among individuals but generally includes the following aspects:
- Joint pain: Rheumatoid arthritis (RA) symptoms can affect a wide range of joints throughout the body, including the fingers, wrists, shoulders, elbows, hips, knees, ankles, and toes. Among these, the fingers and hands region is often the most commonly affected joint. The typical symptom is joint pain, which can vary from constant to intermittent. This pain is typically more pronounced in the mornings or after extended periods of inactivity, as is stiffness. The initial stage of symptoms, called early RA, can be mild and often overlooked, but it is recommended that if you have joint pain or stiffness that persists over the days, see your doctor to determine its origin (5).
- Morning stiffness: Patients with rheumatoid arthritis often experience joint stiffness upon waking up in the morning, which can last for more than an hour.
- Swelling and heat: In disease flares, the affected joints may be swollen, warm to the touch, and reddened due to inflammation, in addition to pain.
- Fatigue: Many patients with rheumatoid arthritis experience chronic fatigue, which can be debilitating and affect their quality of life.
- Joint deformities: Chronic inflammation can lead to joint deformities over time, especially in the hands and feet.
- Systemic symptoms: Some patients may experience systemic symptoms such as fever, weight loss, and muscle weakness.
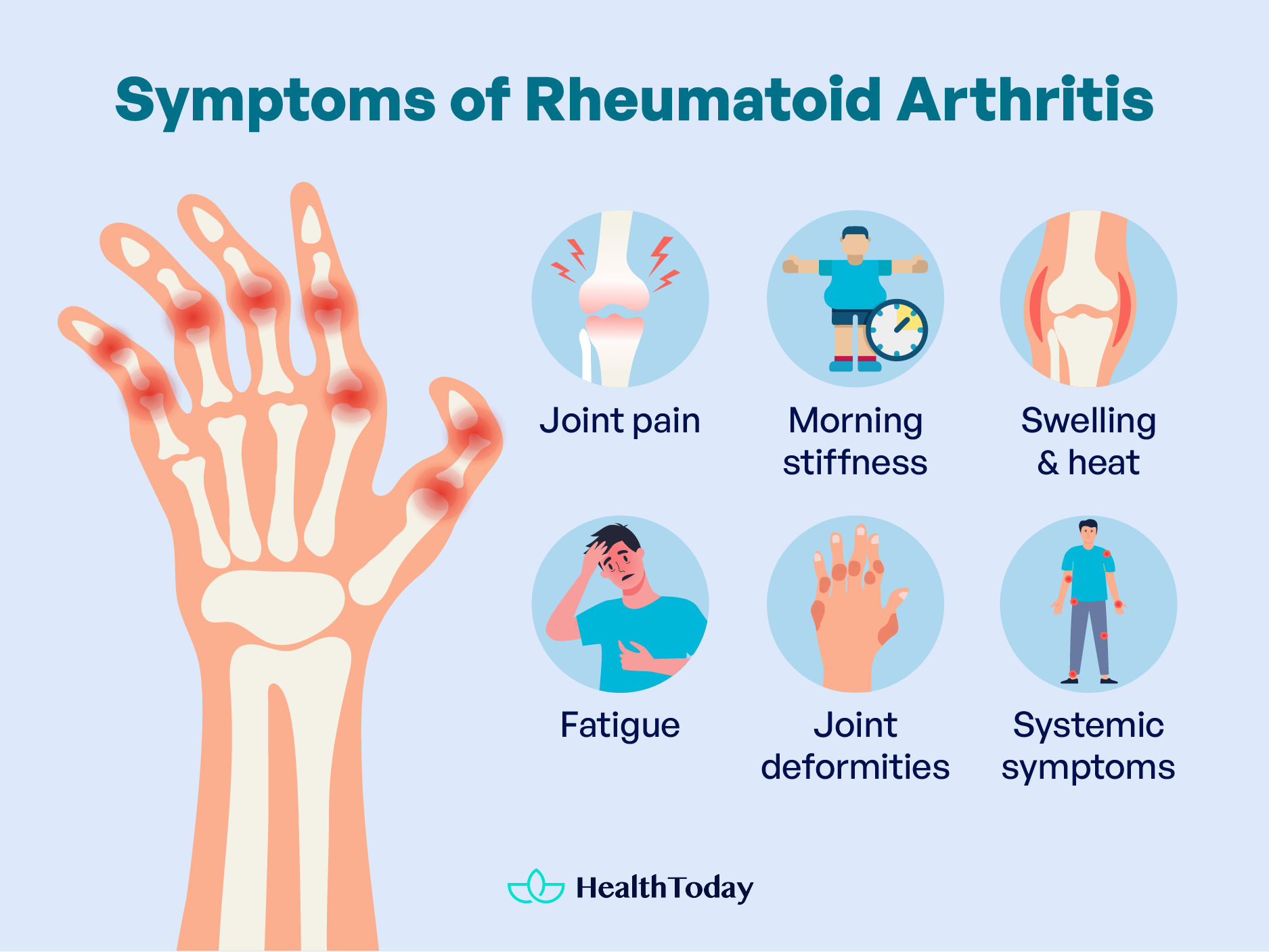
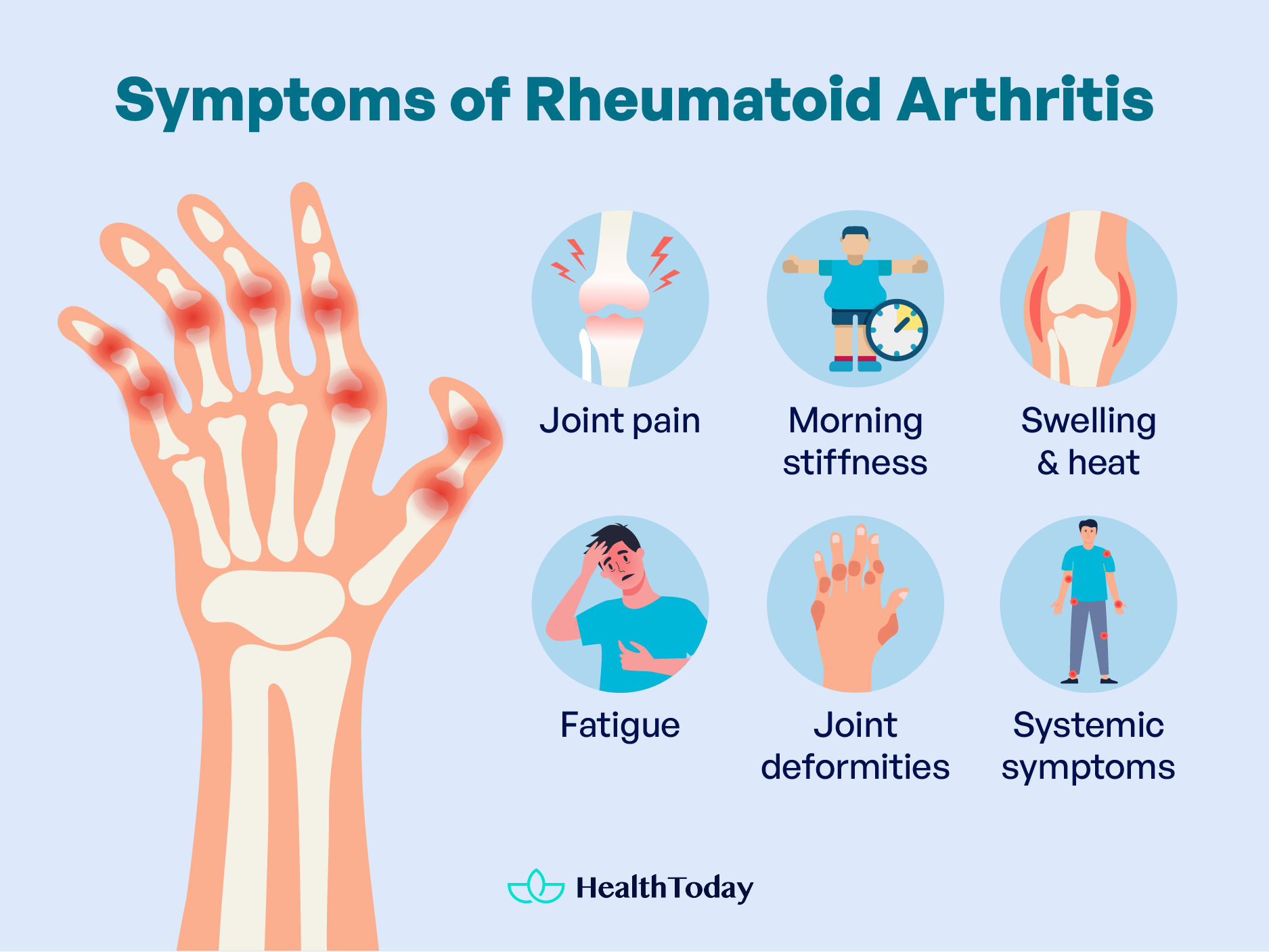
It is important to note that rheumatoid arthritis can vary in severity and clinical presentation among individuals and that early diagnosis and treatment are crucial for controlling symptoms and preventing irreversible joint damage.
What can RA do to your body?
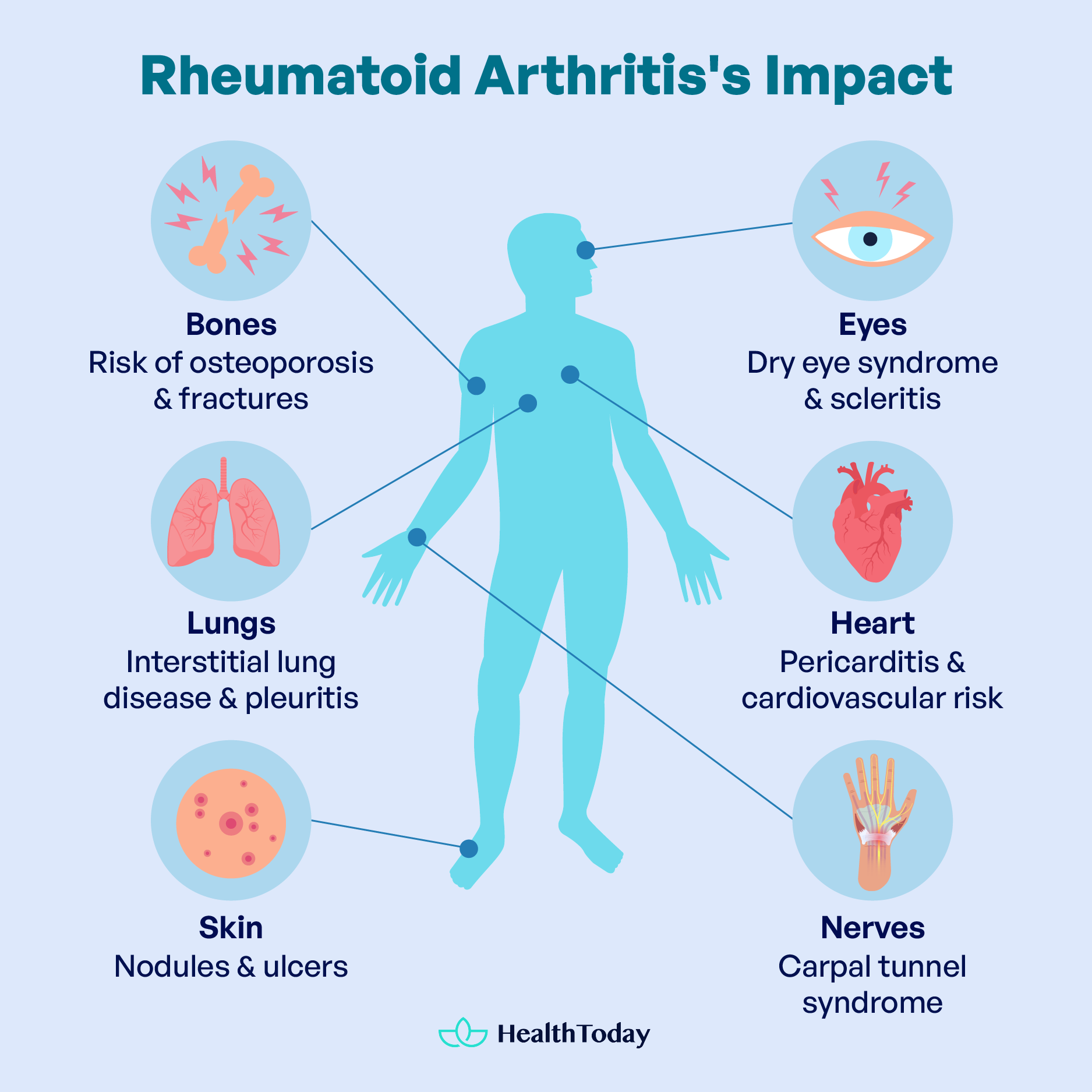
Rheumatoid arthritis, due to chronic inflammation, can affect several organs in addition to joints, such as:
Bones
Rheumatoid arthritis can lead to osteoporosis due to chronic inflammation, as well as from the use of glucocorticoids without medical supervision. Osteoporosis is a disease in which bones become fragile and prone to fractures due to loss of bone density.
Glucocorticoid therapy may increase the risk of osteoporosis by interfering with the normal balance between bone formation and bone resorption. It is crucial that patients receiving glucocorticoids for the treatment of rheumatoid arthritis be closely monitored by healthcare professionals, and strategies to prevent bone loss, such as calcium and vitamin D supplementation and regular physical exercise, should be considered (6, 7).
Skin
Rheumatoid nodules may develop under the skin, especially in pressure-prone areas like elbows and knees. Ulcers can also appear due to multiple factors, such as an alteration in circulation due to inflammation of the vessels. These occur most frequently in the legs.
Eyes
Rheumatoid arthritis damages the connective tissue that covers the ends of the bone joints. This tissue is composed of collagen, the main component of the sclera and the cornea (8).
Inflammation of the eye components leads to a condition called dry eye syndrome or keratoconjunctivitis sicca. In simpler terms, the main symptom is dry eyes, which cause discomfort and a sensation of a foreign body in the eye.
Another condition it may cause is scleritis, particularly in adults aged between 40 and 70 years. This occurs because inflammation thins the sclera or the eye wall. Symptoms include redness of the eye (even after using eye drops), pain, and sensitivity to light.
Glucocorticoids can help control inflammation in eye problems. However, it’s important to note that the use of steroids, as well as the inflammation they treat, can lead to other eye problems if not closely monitored by a healthcare professional.
Lungs
One of the most common pulmonary conditions related to rheumatoid arthritis is interstitial lung disease (ILD), also known as pulmonary fibrosis (9). In ILD, chronic inflammation causes scarring in the lung tissues, making breathing difficult and leading to coughing and fatigue. Although ILD may be asymptomatic in its early stages, it can cause significant respiratory difficulties and reduce lung capacity over time.
In addition to ILD, rheumatoid arthritis can also increase the risk of other lung conditions, such as pleuritis, which is inflammation of the membrane that covers the lungs and the inner lining of the chest. Pleuritis can cause chest pain when breathing deeply.
It is important to note that not all people with rheumatoid arthritis will develop pulmonary problems, and the severity of these manifestations can vary widely from one individual to another. However, it is essential for people with rheumatoid arthritis to be aware of the possibility of lung problems and to communicate with their doctor if they experience respiratory symptoms such as difficulty breathing, persistent cough, or chest pain.
Heart
Regarding heart health, RA can cause inflammation of the pericardium, the layer surrounding the heart, resulting in a condition called pericarditis (10). Usually, pericarditis does not produce symptoms, but it can sometimes cause chest pain that worsens with breathing.
Rheumatoid arthritis increases the risk of developing cardiovascular problems such as heart disease and strokes by causing chronic inflammation in the body (11). However, appropriate treatment that helps control the disease can reduce this risk and decrease the chance of serious complications.
Nerves
In rheumatoid arthritis, it is common to experience compressions of the peripheral nerves in areas such as the wrist, which can cause carpal tunnel syndrome due to inflammation of the synovial membrane. In more advanced stages, joint deformities can also lead to nerve compression. Typical symptoms include numbness, tingling, muscle weakness, and pain in the hands.
People with rheumatoid arthritis must consult their doctor upon noticing the first symptoms to control inflammation and prevent damage to the peripheral nerves.
Living with Rheumatoid Arthritis
Medical treatment for RA typically involves the use of drugs such as NSAIDs to manage pain, glucocorticoids to reduce inflammation, and specific disease-modifying drugs that slow joint damage. However, alongside medication, lifestyle habits play a significant role in effectively managing rheumatoid arthritis. It is recommended to (12, 13, 14):
- Engage in regular physical activity: Exercise is a fundamental tool for improving joint function, relieving pain, maintaining flexibility, and strengthening surrounding muscles. It also helps prevent osteoporosis, a common complication in people with rheumatoid arthritis.
- Eat a varied and balanced diet: Although there is no evidence that a specific diet can change the course of the disease, a diet rich in nutrients essential for bone health is recommended. This includes foods such as fatty fish (tuna, salmon, sardines), egg yolk, dairy products, green leafy vegetables, and legumes (chickpeas, lentils, white beans). This diet, high in vitamin D and calcium, helps prevent osteoporosis, which is especially important due to the chronic use of glucocorticoids in treating rheumatoid arthritis.
- Maintaining a healthy body weight: Maintaining an appropriate weight helps prevent disease complications and reduces the burden on affected joints. In addition, it can improve response to treatment and overall quality of life.
- Avoid smoking: Smoking is not only a risk factor for the development of the disease but has also been associated with a worse course and response to treatment in people with rheumatoid arthritis. Smoking cessation can significantly improve prognosis and quality of life and reduce the risk of heart disease.
- Managing stress and emotional aspects: Reducing stress and addressing the emotional aspects associated with the disease can help patients deal with it more amenably. This promotes better adherence to treatment and self-care habits.
By adopting these healthy lifestyle habits, people with rheumatoid arthritis can improve their quality of life, reduce the risk of complications, and optimize long-term disease management.


Is rheumatoid arthritis pain constant?
Rheumatoid arthritis (RA) pain can vary from person to person. Some individuals may experience constant pain, while others may have periods of remission where pain is minimal or absent. RA pain tends to be worse during flare-ups when inflammation levels are high.
Can arthritis cause poor circulation?
Arthritis itself typically does not directly cause poor circulation. However, certain arthritis-related complications, such as vessel inflammation or joint damage, may indirectly affect circulation in some cases.
Is rheumatoid arthritis chronic?
Rheumatoid arthritis (RA) is a chronic autoimmune disorder. It is characterized by inflammation in the joints, leading to pain, stiffness, and potential joint damage over time. RA requires ongoing management and treatment to control symptoms and prevent disease progression.
Can you live with RA without medication?
While it’s possible to manage rheumatoid arthritis (RA) without medication through lifestyle changes, such as diet and exercise, medication is typically necessary to effectively control symptoms, prevent joint damage, and improve quality of life.
Do arthritic joints hurt when pressed?
In many cases, arthritis can indeed cause pain when the affected joint is pressed or touched. This pain may vary depending on the type and severity of arthritis, as well as individual factors such as pain tolerance.
What causes rheumatoid arthritis to get worse?
Several factors can contribute to the exacerbation of rheumatoid arthritis (RA) symptoms, including inadequate treatment or medication adherence, ongoing inflammation, autoimmune activity, progressive joint damage, lifestyle factors such as stress, poor diet, and lack of exercise, as well as coexisting medical conditions or complications.
Summary
Rheumatoid arthritis (RA) is a chronic autoimmune disease affecting millions of people worldwide. It is characterized by joint inflammation, pain, and stiffness, and certain systemic effects, such as fatigue, sometimes accompany it. Although its exact cause is not yet fully understood, there are risk factors that increase the likelihood of developing the disease, such as family history, being overweight, female gender, and smoking.
The diagnosis of RA is based on clinical evaluation by the physician, as well as laboratory tests. X-rays of the affected joints may also help confirm the diagnosis.
Treatment of RA usually involves the use of medications, such as nonsteroidal anti-inflammatory drugs to relieve pain, glucocorticoids to reduce inflammation, and specific disease-modifying drugs. In addition, lifestyle changes are recommended, such as maintaining a healthy weight, avoiding smoking, and following a balanced diet and regular exercise. These habits can improve joint function, reduce pain, and prevent complications such as osteoporosis, thus improving the quality of life of people with RA.
Early diagnosis and treatment are essential to control symptoms and prevent irreversible joint damage. People with RA must have adequate medical follow-up to develop a treatment plan and adopt a comprehensive approach to disease management.

















Comments
0