Table of Contents
Picture this: mornings greet you with a bitter or sour taste, chest discomfort, or a cough. Acid reflux when sleeping can be the reason behind these unwelcome morning surprises.
If acid reflux is left untreated, it can evolve into gastroesophageal reflux disease (GERD), which can even lead to cancer. However, falling for “online GERD fixes” can bring more persistent or worsening nighttime symptoms. So, figuring out how to sleep with GERD symptoms at night is a big win for your health.
Acid reflux when sleeping: Causes and symptoms
Experiencing acid reflux in sleep is often more severe and challenging to manage than during the day.
What is GERD and acid reflux?
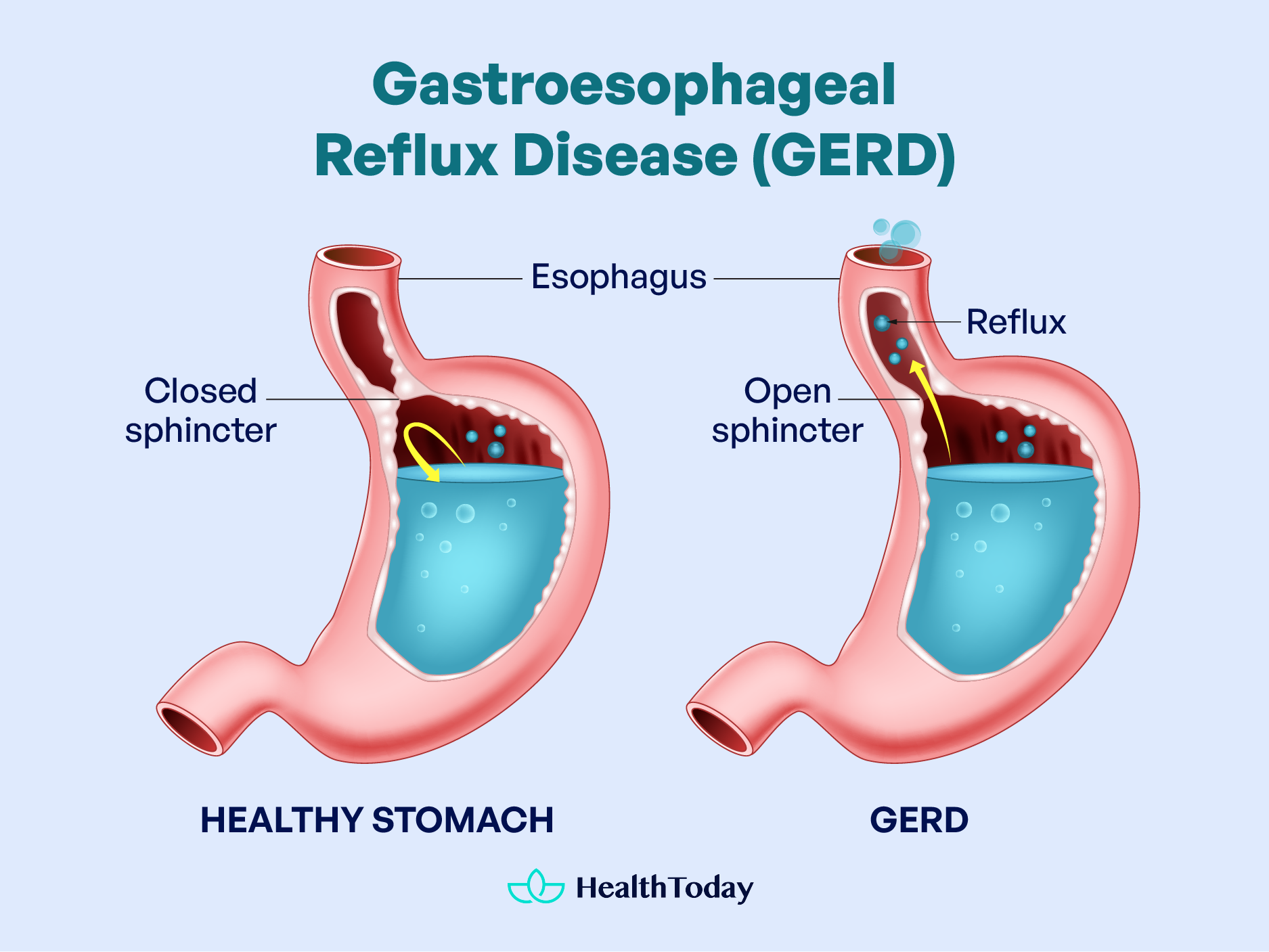
Acid reflux, or gastroesophageal reflux (GER), occurs when stomach acid flows back into your esophagus, causing irritation (1).
Everyone can experience reflux when eating triggering foods. In most cases, it’s mild, occasional, and resolves quickly. But suppose it occurs regularly, like twice a week. In that case, you may have gastroesophageal reflux disease (GERD), a more severe and lasting condition (1, 2).
In the US, over sixty million people (20% of the population) have GERD. About 10-20% of persons with GERD will go on to develop Barrett’s Esophagus, a condition that involves chronic inflammation of the esophagus and a precursor to esophageal cancer. (3, 4).
Symptoms of GERD
GERD patients often have symptoms both during the day and at night. It’s rare to find someone who deals with just one or the other (5).
The two classic GERD symptoms are heartburn (a painful burning sensation below or behind the breastbone) and regurgitation (a bitter or sour taste in your mouth). These symptoms usually impact the lower esophagus in your chest (6, 7).
Heartburn may worsen after meals, disturb sleep, or be sparked by exercise, resembling chest pain from heart disease. Symptoms may last minutes or hours and often get better with antacids or acid-suppressive medications (7).
In more severe GERD cases, the refluxed content can reach your larynx (voice box), pharynx (throat), and even lungs after escaping into the mouth. The medical term for this is laryngopharyngeal reflux (LPR) (8).
LPR is also known as “silent reflux,” as it may not cause heartburn but often irritates your voice, throat, and sinuses (8, 9). About 20% of GERD cases may have silent reflux, leading to millions of delayed or missed GERD diagnosis. For example, chronic cough can be the sole symptom in more than 50% of GERD cases (7, 10).
Other symptoms of LPR are (7, 8, 10, 11):
- Chest pain
- Shortness of breath
- Bad breath
- Nausea
- Bloating
- Difficulty or painful swallowing (dysphagia)
- Sore throat
- Hoarseness
- Wheezing
- A feeling of a lump being stuck in your throat (Globus sensation)
- Waking up at night with burning in the throat or a choking sensation
- Frequent throat clearing
- Phlegm or excessive mucus
- Postnasal drip
- Nagging or chronic cough (defined as cough for three weeks)
- New or worsening asthma
If you experience any of these symptoms for more than two weeks, it’s important to see a doctor. However, for chronic cough, it is typically described as three weeks before needing to see a doctor (7, 10).
When seeing your doctor, consider asking them to check for reflux conditions. A lack of basic acid effects like heartburn may suggest that repeated acid exposure has numbed your esophagus. In such cases, respiratory symptoms should be viewed as a serious alarm for potential esophageal damage (10).
Possible causes of GERD
You are at a higher risk of GERD if you (6, 12, 13):
- Experience delayed gastric emptying.
- Are overweight or obese, or have diabetes. These conditions can put more strain on your stomach.
- Are pregnant. Pregnancy can trigger or worsen heartburn due to an increase in hormones like progesterone and estrogen (2, 11).
- Smoke, or are regularly exposed to secondhand smoke.
- Have hiatal hernia, when the upper part of your stomach pushes through your diaphragm, moving up into your chest.
- Take certain medications.
These conditions can increase belly pressure, affecting a muscle band called the lower esophageal sphincter (LES). This band seals off the esophagus when food or liquid enters your stomach (6). If the LES weakens, relaxes, or doesn’t close tightly, stomach acid or food can return to the esophagus, causing a reflux episode (2, 12).
A surprising cause of acid reflux is insufficient stomach acid (hypochlorhydria). Hypochlorhydria can result in poor digestion, allowing gas bubbles—carrying stomach acid—to travel into your esophagus and throat. Even a small amount of acid in your throat can be distressing (10, 14).
Why is GERD worse when lying down?
Recent research suggests that compared to people with daytime GERD, nighttime GERD patients tend to have more severe symptoms, including nightmares, frequent awakenings, choking, and coughing up stomach acid at night (5, 15, 16). This can be traced back to prolonged acid contact time caused by:
- Lack of gravity support: Normally, gravity helps prevent stomach contents from flowing back when standing or sitting. Gravity no longer helps keep stomach acid down when you lie down (9, 17).
- Circadian rhythm: The secretion of gastric acid peaks between 10 PM and 2 AM (16).
- Swallowing less: There’s less force pushing stomach acid downward (17).
- Less saliva: During deeper sleep stages, less saliva is produced, and saliva helps neutralize stomach acid (17, 18).
- Sleep disturbances: Sleep deprivation in GERD patients results in increased sensitivity to acid (19).
- Medicine: Medications for sleep disturbances can relax LES (2, 20).
The link between GERD and obstructive sleep apnea
Obstructive sleep apnea (OSA) occurs when the throat walls relax and narrow during sleep, interrupting normal breathing and leading to sleep disruptions (21). Studies indicate that around 58 to 62 percent of patients with OSA may have GERD (17, 22). However, it may be related because both populations tend to have higher rates of obesity.
Recently, there’s been emerging evidence supporting the link between GERD and obstructive sleep apnea. GERD may impact breathing, causing more nighttime apneas, while OSA can affect gastric function and pressure in GERD (17, 19, 22, 23).
A study involving 65,333 participants revealed that people with GERD symptoms had about three times higher likelihood of experiencing insomnia and sleeplessness (24).
In a survey of 1000 adults with heartburn, 79 percent reported having nighttime heartburn. Among them, 75 percent said it affected their sleep, and 40 percent believed it impacted their functioning the next day (25).
Treatments for GERD have been shown to improve sleep quality, and addressing sleep disorders can ease nocturnal GERD symptoms (23, 27). While more research is needed to understand the exact link between GERD and OSA, it’s clear that these conditions can coexist, posing substantial challenges to sleep, comfort, and overall health.
GERD usually brings two main symptoms: heartburn and regurgitation. But watch out for silent reflux, a quieter player in 20 percent of cases, often mistaken for other respiratory problems. Plus, GERD often becomes worse when lying down, potentially causing obstructive sleep apnea.

Does GERD cause stomach pain?
Some people with GERD may experience stomach pain or discomfort. This is because a weakened LES allows stomach acid to irritate the stomach lining, leading to extreme GERD pain. Having a hiatus hernia might make the pain worse (28).
Heartburn, a burning feeling under the breastbone, is also a discomfort due to the regurgitation of stomach acid. Heartburn can sometimes be mistaken for GERD-related abdominal pain or stomach pain since these organs are close. The pain might also reach the back, neck, jaws, throat, or arms (2, 7).
Stomach pain can be caused by various conditions, not just GERD. Some less common ones include (28):
- Indigestion and irritable bowel syndrome (IBS)
- Gastritis, appendicitis, or pancreatitis: Inflamed stomach lining, appendix, or pancreas
- Gastric ulcer: Erosion of the stomach lining
- Pneumonia: Lung infection
- Gallstones/kidney stones
- Heart attack
- Menstrual cycle pain
What happens if nighttime GERD is untreated?
Repeated reflux over an extended period—both daytime and nighttime—can trigger issues in the lower part of the esophagus, including (9):
- Inflammation (esophagitis), including erosive esophagitis (acid-induced) and eosinophilic esophagitis (allergies response) (29)
- Scarring
- Narrowing (stricture)
- Ulcers (disruptions of the inner surface)
- Barrett esophagus, or changes to the esophageal cell lining, affects 10 to 20 percent of GERD patients. The main concern is that Barrett’s esophagus is a big risk factor for esophageal adenocarcinoma, a deadly cancer (4, 30).
- Esophageal cancer
Persistent GERD raises the risk of respiratory infections, such as pneumonia and asthma, as refluxed contents enter the lungs (10, 12, 31). When the acid reaches the mouth, it can cause dental problems like enamel erosion and tooth decay (32).
Long-term GERD may also trigger bleeding from ruptured blood vessels (12), causing vomited blood, dark stools (melena), or bright red blood in the stool. Long-term bleeding may result in iron deficiency anemia (9).
Continuous lack of sleep from GERD may increase the risk of developing (33):
- Dementia
- Heart disease
- Type 2 diabetes
- Obesity
- Cancer of the breast, colon, ovaries, and prostate
Inadequate sleep can also affect daily tasks by impairing memory and concentration and increasing stress and anxiety levels (33, 34).




Sleeping with GERD: Top tips for relief
Managing GERD is not a one-time action; it’s more of a consistent habit.
Let’s check out some simple sleep techniques for GERD, which can make a real difference in reducing how often and how strong flare-ups happen!


Myth debunked: Will boosting acid help with GERD?
Stomach acid is vital for digestion, and without it, gastric emptying takes longer, letting gas bubbles move into the esophagus and throat and causing acid reflux (14). So, some “online tips” suggest that enhancing stomach acid may aid in easing GERD.
These “acid hacks” involve taking stomach acid supplements like betaine or acidic and tangy foods, such as apple cider vinegar or citrus drinks (35, 36). However, these “supplements” have yet to be scientifically proven effective. The truth is that they could backfire and make GERD worse by activating an enzyme called pepsin.
Pepsin, the enzyme that helps digest proteins, moves up with stomach contents during reflux. Pepsin can attach to organs—such as the throat and esophagus—and linger there for a long time. As our cells are protein-based, pepsin can “digest” them, causing prolonged oxidative stress, heartburn, inflammation, and potentially esophageal cancer (10, 37, 38, 39).
Pepsin often alternates between active and “sleep” modes. At pH seven, it remains in its inactive form, pepsinogen, and becomes more active with a lower pH. Consuming acidic foods can easily wake up pepsin, leading to more inflammation and cell damage. This is akin to pouring acid on a wound (38, 39, 40).
What to eat?
Reflux at night can respond well to some simple daytime diet tweaks, focusing on maintaining gastric acidity at a pH of 4.0 or higher (10, 16). So, which foods are a no-go with GERD? We’ve got the list for you (2, 10, 11, 41):
- High-fat foods, including full-fat dairy products
- Junk foods and processed foods, even canned vegetables or baby foods. Here is a simple rule to keep in mind: The more processed the food, the more it can worsen acid damage since it contains trans fats and is acidified for preservation. So, home cooking is a key to preventing acid reflux in sleep.
- Sugary foods, especially foods containing high-fructose corn syrup (HFCS). The bacteria causing reflux thrives on sugar, and HFCS is more harmful as it contains sulfuric acid, an extremely acidic substance (10).
- Spicy and strong-smelling foods: chili, raw onion, raw garlic
- Alcoholic drinks: beer, wine, distilled spirits
- Minty flavors: mint, peppermint, spearmint, toothpaste, and peppermint tea
- Caffeine-containing foods: coffee, tea, chocolate, soda (42).
- Acidic fruits and juices: citrus, orange, lemon, lime, pineapple, tomato, and tomato sauce
- Carbonated beverage, including flavored seltzer water. With a pH of about 2.5, soda is the most acidic, sleep-disturbing, and corrosive substance people often consume (10).
These foods increase acid secretion, delay stomach emptying, increase acid exposure, or loosen the LES (43, 44). So, instead of eating these foods, you can opt for lean proteins, whole grains, and fiber-rich foods (43, 45). The superfoods for GERD are (12):
- Bananas, being alkaline, are considered to help neutralize stomach acid (46). Fresh bananas can create a protective coating on the delicate esophageal lining, strengthening the defenses against reflux. Bananas also contain pectin, a soluble fiber that helps keep a smooth flow of food through the digestive tract.
- Oats are high in fiber and well-tolerated, giving them a soothing effect.
- Almonds, being rich in healthy fats, can neutralize stomach acid.
- Green leafy vegetables like spinach, broccoli, kale, asparagus, and Brussels sprouts are naturally low in fat and sugar and packed with antioxidants to prevent inflammation caused by acid.
- Legumes, a healthy fiber and protein source, can speed up transit time and prevent constipation (10, 47).
- Lean protein is essential for a healthy diet. However, it’s important to consume red meat in moderation and opt for poultry and meat (10).
- Omega-3 fatty acids, which have anti-inflammatory effects, found in fatty fish or flaxseeds, may have therapeutic potential for GERD (48).
Home remedies
Besides eating the right foods, some herbal remedies are helpful for nighttime heartburn, according to Harvard Medical School (49):
- Chamomile or chamomile tea, being known for its calming properties, can help reduce inflammation and relieve GERD symptoms (12, 50)
- Ginger, with its anti-inflammatory properties, may inhibit gastric acid production (51). Ginger’s prokinetic, or digestion-promoting, activity has been confirmed in tests (50).
- Deglycyrrhizinated licorice (DGL) is a form of licorice root. This root can inhibit an enzyme called H+/K+ ATPase, which is involved in acid secretion (52).
- Marshmallow root and slippery elm contain mucilage, which forms a gel-like coating on the delicate lining of the esophagus, acting as a barrier against acid (12).
- Papaya or papaya juice, containing digestive enzymes like papain, supports healthy digestion and reduces GERD symptoms (12, 53).
- Turmeric, which contains curcumin, has potent anti-inflammatory effects, and can reduce the inflammation effects of reflux (54, 55). Curcumin can also reverse pepsin’s damaging effects (37).
Other remedies, such as catnip, aloe vera, verum, and fennel, have historical use, but scientific evidence is limited (49, 56, 57). Herbal remedies often lack FDA approval, so it’s best to consult your healthcare provider before trying them (49).
How to Eat?
Preventing discomfort due to the regurgitation of stomach acid at night is not just about the food; it’s also about how you enjoy it. Here are some essential eating tips to make your nights more peaceful (41, 11, 10, 58):
- Avoid eating within 3–4 hours of bedtime. This is important because emptying your stomach takes about three to four hours (10).
- Eat smaller, frequent meals to avoid overeating or going hungry for extended periods, which can overload the LES (59). Also, enjoy your meal slowly and calmly, separate from work and distractions.
- Stay upright for at least an hour after meals and avoid excitement. If you sense reflux, have a glass of water.
- Chew sugarless gum after meals to increase saliva, neutralize acid, soothe the esophagus, and wash acid back into the stomach. Avoid peppermint-flavored gum, which may trigger heartburn.
Get better sleep


Tips for better sleep often align with managing GERD, such as avoiding smoking, caffeine, and alcohol. Enhance your sleep experience with these additional GERD-friendly tips (2, 10):
- Sleep with your torso elevated about 6 inches (15 centimeters). You can use a wedge-shaped pillow under your mattress. Avoid using too many pillows because they are less effective and can slip at night. Also, regular pillows may be ineffective, as they elevate only your head and not your upper body. If possible, you can lower the foot of your bed (58).
- Don’t wear clothes that are tight around your waist. They can squeeze the stomach, pushing its contents into the esophagus. Losing weight is also helpful if you’re overweight.
- Research suggests that sleeping on your left side is the optimal position for GERD because it helps clear acid faster (60, 61). If maintaining this position is a challenge, consider using a sleep-positioning device (SPD) for added support (62).
- Practice good sleep hygiene. This involves creating a quiet, dark, and cool bedroom. Calming sounds—like rainfall, gentle music, or white noise—can also be helpful for sleep (63).
- Maintain a set schedule for going to bed and waking up. Ideally, follow the same sleep routine every day, even on weekends (63).
- Try diaphragmatic breathing exercises, or abdominal breathing, that strengthen diaphragm tendons near the LES, creating a stronger barrier against acid reflux (10, 64)
Anxiety, worry, and stress can impact your sleep and GERD symptoms. If this applies to you, trying relaxing hobbies and stress-busting techniques—such as meditation and tai chi—into your routine is a good idea (11, 65). If you find yourself often worrying in bed, allocating time before sleep to create a to-do list for the next day can help you unwind (63).
Exercise
Moving more is good for your weight management, gastric motility, and stress hormone, a big combo that tackles acid reflux in sleep (10, 66). This is particularly important if you sit a lot during the day, which has been called the “new smoking” due to its connection to a higher risk of inflammation and cancer (10, 85).
However, special precautions are needed for exercising with GERD.
In one study, running prolonged esophageal acidity and increased the frequency and duration of reflux episodes in healthy athletes (68). So, it’s best to avoid vigorous exercise involving jumping, intense abdominal workouts, or being upside down (such as headstands).
In most cases, you can opt for low- to moderate-impact cardio exercises like brisk walking and low-impact yoga. A simple tip is taking a nighttime walk to reduce bedtime reflux (10).
Pay attention to how you feel during exercise, as tolerance varies. It’s best to exercise at least 90 minutes before bedtime and two hours after eating or consider a morning workout (10, 58, 63).
Fortunately, intense workouts are not necessary for exercise benefits. Regularity is more important than intensity, as the positive effects don’t last long (10).
The minimum recommended exercise is 150 minutes per week, or around 21 minutes a day. It’s better to spread these minutes throughout the week rather than cramming them into one day. This approach will preserve the mood-boosting perks of exercise and energize you (10, 69).
Remember to warm up before exercising and cool down afterward. Stay hydrated by drinking 16 ounces (2 cups) of water upon waking before exercise (10). However, avoid certain sports drinks as they can be highly acidic (70).
Over-the-counter (OTC) medications
If you’re still not fully relieved with the methods above, consider GERD medications that are available over the counter (2, 71):
- Antacids (e.g., Maalox, Mylanta, or Tums): They neutralize stomach acid and are often used for mild GERD symptoms. However, it’s important not to use them daily without consulting your doctor, which can make reflux worse by prompting more stomach acid production and triggering diarrhea or constipation (71, 72).
- H2 Blockers, such as Famotidine (Pepcid AC), Cimetidine (Tagamet HB), and Nizatidine (Axid AR): They reduce stomach acid production to aid in esophageal healing.
- Proton pump Inhibitors (PPIs), like Omeprazole (Prilosec OTC or Zegerid OTC), Lansoprazole (Prevacid 24 HR), and Esomeprazole (Nexium 24 HR): They nearly stop all stomach acid production. Thus, they are more effective in treating GERD symptoms than H2 blockers. However, PPIs still have limitations due to slow onset and short duration (27). Also, long-term use of PPIs is linked to increased overall mortality, kidney issues, upset stomach, and foodborne infections (12, 71, 73).
- Potassium-competitive acid blockers (P-CABs), like Tegoprazan: They offer faster action and longer effectiveness for GERD than PPIs (27). They are now available in some countries but not in the US.
- Melatonin: It is a hormone produced by the body to promote sleep. This hormone might also protect the esophagus in people with GERD and heartburn. Research indicates that melatonin could be as effective as a PPI in improving GERD (74).
- Alginates, such as Gaviscon: This drug creates a protective barrier in the stomach to help prevent acid reflux (75).
- Prokinetics, like Metoclopramide: They are used to improve gastric emptying and upper gut motility (12, 76). Prokinetics can be added to a PPI regimen but are not as effective on their own (9).
Healing usually requires taking these drugs for 4 to 12 weeks (9). For people with respiratory symptoms, it might take longer for all throat inflammation to resolve. In asthma patients, it could take up to 3 months of treatment to see improvement in bronchial symptoms (7).
Medicines Regulation
Certain medications can cause or worsen GERD symptoms (2, 6, 11):
- Sedatives that promote calmness or sleepiness, such as benzodiazepines and non-benzodiazepine hypnotics (17)
- Calcium channel blockers or beta-blockers, used to treat high blood pressure
- Certain asthma and lung medications like bronchodilators, theophylline, beta 2-agonists, and prednisone (7)
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for inflammation or pain, such as ibuprofen
- Tricyclic antidepressants for stress and anxiety
- Anticholinergics used for sea sickness
- Dopamine-like drugs for Parkinson’s disease
- Progestin for abnormal menstrual bleeding or birth control
When to See a Doctor?
If you notice having a reflux, seek immediate medical attention if (2):
- You vomit material that is bloody or resembles coffee grounds.
- Your stools are black (like tar) or maroon.
- You experience a burning sensation and a squeezing, crushing, or pressure in your chest, especially with shortness of breath. Sometimes, those who believe they have heartburn may be having a heart attack (90).
It’s also important to call your doctor if (2, 6, 11):
- You experience heartburn most days or if it persists despite self-care efforts.
- You unintentionally lose weight.
- Swallowing becomes difficult (food feels stuck).
- You lose your appetite or vomit.
- Persistent cough or wheezing occurs.
- Your reflux symptoms worsen with OTC medicines.
- You suspect one of your medications may be causing heartburn. Don’t change or stop taking your medicine without consulting your doctor or pharmacist.
Your doctor can thoroughly assess the situation, order relevant tests, and suggest appropriate treatment (77).
In cases where lifestyle changes and medications don’t improve GERD symptoms, or if you prefer not to take long-term medications, your doctor might recommend surgery. However, these procedures have higher risks and are not commonly used (71).




What causes acid reflux to flare up?
Is there any instant relief for GERD?
There is no quick fix for GERD. The symptoms hang around because of long-term tissue inflammation due to acid exposure. So, whatever treatment you choose, give your tissues the time they need to heal completely (10).
Can water calm GERD?
Can GERD heal naturally?
Does walking help acid reflux?
Yes, walking speeds up digestion, helping empty and shrink the stomach faster, reducing the risk of reflux. It’s best to make post-dinner strolls a regular habit for your reflux, sleep, and mental health (10).
Summary
GERD usually brings two main symptoms: heartburn and regurgitation. GERD symptoms at night are often worse than daytime GERD, potentially disrupting your sleep.
How to sleep with GERD? Rather than using medications with potential side effects, focus on addressing root causes by avoiding food and habit triggers. You can also try proven remedies, but be careful that some “online therapies,” like eating acidic foods, may worsen GERD.
Include exercise and stress-reducing techniques in your routine, as it can improve sleep, increase energy, and enhance motivation to stick to your dietary goals.
















Comments
0