Table of Contents
Can eating sugar cause diabetes? This question emerges in the continuing discussion of sugar’s effects on our health. Join us to find out the answer and details of how much sugar can cause diabetes.
Artificial sweeteners, offering a sweet taste without calories, are the perfect choice for weight loss and are safe for your health? How much of this is true? Let’s sift through the facts and myths behind the sweet speculation.
Does eating sugar cause diabetes? Facts to know
The short answer to “Does sugar cause diabetes?” is no, it does not directly cause diabetes. However, increased sugar intake is associated with an increased risk of type 2 diabetes.
Diabetes is a chronic disease triggered by many factors (1). So, whether it’s type 1, type 2, or other types of diabetes, sugar is not the sole reason, but too much of it can raise the risk for certain diabetes types.
How is sugar metabolized in your body?
‘Sugar’ is often referred to as table sugar or sucrose, composed of one glucose molecule and one fructose molecule (2, 3).
Sugar (glucose) is a main source of energy for our body, fuel for our brain, muscles, heart, and overall health (4, 5). Dietary sugars are absorbed in the liver as glucose, fructose, or galactose (4).
Glucose
Glucose is the body’s main source of energy. Your body will break down the foods you eat, like carbs, lipids, or proteins, into glucose and release it into your bloodstream via the small intestine(5). When your blood sugar increases, your pancreas releases insulin, a hormone that helps glucose enter your cells to be used for energy (4).
It takes a few hours for your cells to absorb glucose and gradually lower blood sugar after eating. Your liver then releases glucose back into the bloodstream to keep things balanced and prevent sugar spikes (5).
Too much sugar makes your insulin overwork, causing insulin resistance (4, 6). Insulin resistance is when cells in your muscles, fat, and liver do not respond well to insulin and can’t easily take up glucose from your blood, resulting in excessive glucose in the blood (7).
When your body has enough energy for functions, the extra glucose becomes fatty acids, stored as triglycerides (lipids) in fat cells, which can cause weight gain (4).
Having high blood glucose for a long time can lead to many health issues (8, 9):
- diabetes
- nerve damage
- heart disease and stroke
- eye problems
- gum disease and other dental problems
- kidney disease
- sexual and bladder problems
- depression and dementia
- sleep apnea
- cancer
Fructose
Fructose, found in many foods such as honey, fruits, vegetables, soft drinks, and processed foods, is mainly processed in the liver, intestines, and kidneys by special enzymes. This process doesn’t need insulin.
Blood sugar levels or insulin won’t increase significantly after a fructose-heavy meal. Yet excess fructose may speed up the body’s use of carbs (4, 10).
In short-term experiments, a high-fructose diet over several days to weeks was not associated with impaired insulin-mediated glucose uptake but with impaired liver insulin sensitivity (4).
When you eat a small amount of fructose, most of it becomes glucose and organic acids in your gut (4, 10), and the liver will store glucose as glycogen.
However, when you eat a fructose-heavy diet (150 grams or more per day), excess fructose can build up in the liver and be converted into fat. This could increase the risk of developing type 2 diabetes and obesity (4, 5).
Excess fructose consumption makes it harder for your body to produce and use leptin, the hunger control hormone (11, 12), which makes you crave more sweet snacks(4).
Galactose
Eating galactose doesn’t raise blood sugar or insulin levels much (4). Your liver metabolizes most of the galactose and turns it into other substances your body needs, like glycogen (4).
However, part of the galactose is released into our bloodstream as free glucose (4). When eating foods that contain galactose, blood triglycerides (for fat cells) may increase, like consuming fructose (13).
Types of diabetes
Every year, 1.5 million Americans find out they have diabetes (5).
When your body doesn’t make enough insulin or insulin doesn’t work well, you are at risk of diabetes (5). It may entail chronic high blood sugar, high blood pressure, and other health problems (8, 14).
Type 1 diabetes is when your pancreas stops making insulin. Over 90% of the cases happen because your immune system kills the cells in the pancreas (5). Sugar doesn’t cause type 1 diabetes, but genes and environmental factors, including viruses, can be the cause (8).
Type 1 diabetes is a chronic disease and often happens to kids. On average, people with type 1 diabetes might live 13 years shorter (5, 8).
Type 2 diabetes is caused by insulin resistance. 95% of people diagnosed with diabetes have type 2 diabetes (5, 9). Lifestyle choices such as less moving and eating unhealthy foods may contribute to developing type 2 diabetes.
Those with a high percentage of fat in their body, or their Body Mass Index (BMI) is in the ‘obese’ zone, are at increased risk of type 2 diabetes (5).
Overeating sugar could worsen insulin resistance and fat buildup by making it harder for the body to use insulin (3).
Gestational diabetes develops during pregnancy, usually diagnosed between the 24th and 28th week (15).
During pregnancy, your body goes through changes and produces special hormones, which can cause insulin resistance. Although most moms can produce enough insulin to overcome it, some can’t, which leads to gestational diabetes (5, 16).
High blood sugar in pregnant women can cause fetal problems for babies, including congenital disabilities, overweight, or stillbirth (5).
Being overweight or having a family history of diabetes is also linked to gestational diabetes (16).
Monogenic diabetes, caused by changes in a single gene, contains some rare forms of diabetes (1‒4% of the cases), often misdiagnosed with type 2 diabetes (17).
In most cases of monogenic diabetes, the gene mutation is passed down from the parents. These mutations may limit the pancreas’s ability to produce insulin (17).
Neonatal diabetes is a subtype of monogenic diabetes affecting the 6-to-12-month-old babies. Another type is maturity-onset diabetes in those ages 20 or younger (17).
No matter which type, sugar is not a direct cause of diabetes, but it can trigger insulin resistance and increase the risk of type 2 diabetes (4).
How much sugar causes diabetes or other risks?
Sugar is not the direct cause of diabetes, so asking, ‘How much sugar does it take to get diabetes?’ might not get you a straight answer. Yet you should know what the limit is.
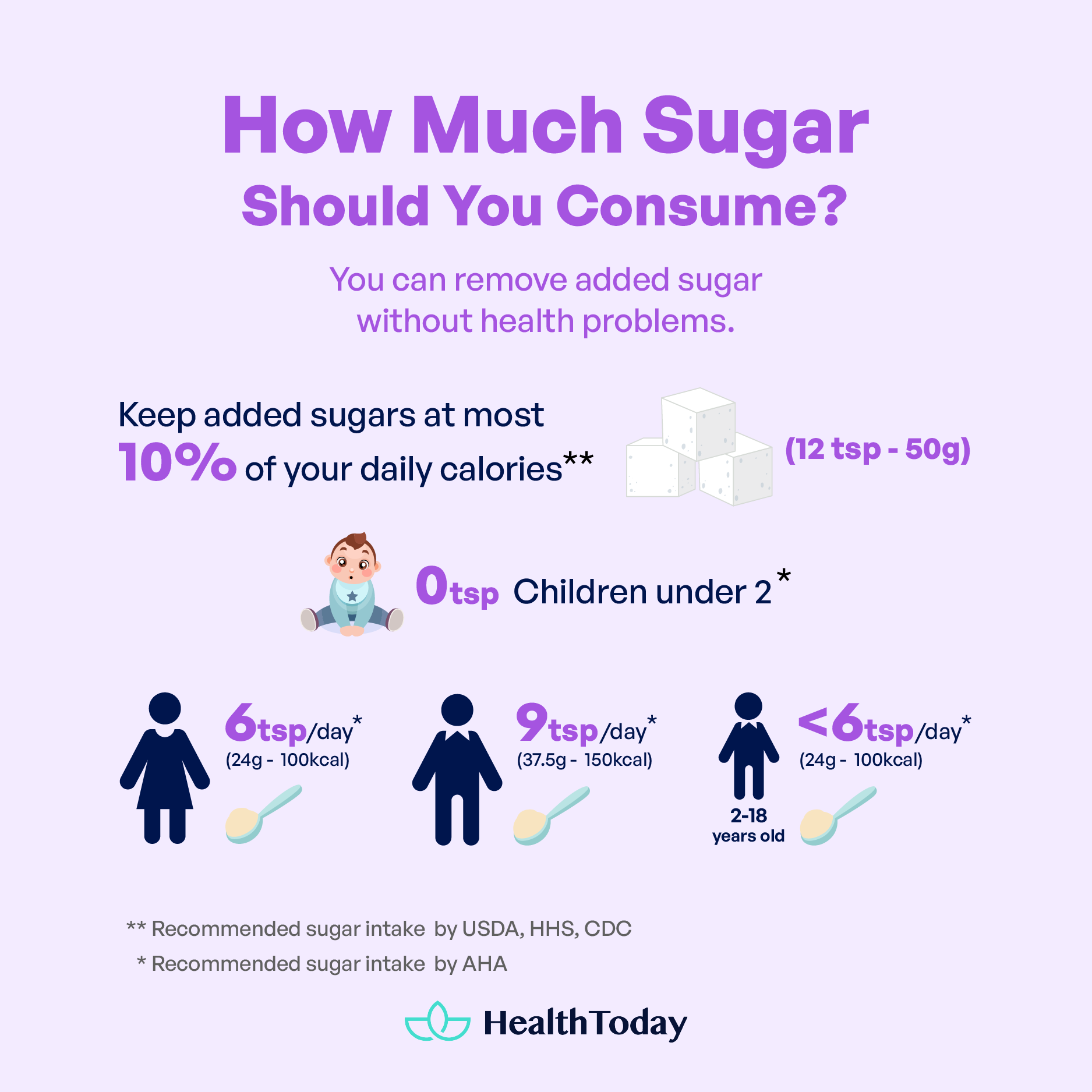
You can eliminate added sugar without any health problems. The Healthy Eating Plate advises using sugary drinks and sweets very little or none (18).
The United States Department of Agriculture (USDA), the Department of Health and Human Services (HHS), and the Centers for Disease Control and Prevention (CDC) also suggest that it’s best to avoid added sugars or (19, 20):
- Keep them at most 10% of your daily calories. For example, if you eat 2,000 calories daily, keep those added sugars under 200 calories. That’s about 12 teaspoons or 50 grams.
- Children under two shouldn’t be given any foods and drinks with added sugars.
The American Heart Association (AHA) also recommends keeping added sugar intake under (21):
- Six teaspoons (about 24 grams, or 100 calories) a day for women
- Nine teaspoons (about 37.5 grams, or 150 calories) a day for men
- Less than six teaspoons a day for children ages 2‒18
- Zero for children under two
Your body uses glucose for energy, but fructose is mainly sent to your liver to be turned into glucose or fat. Insulin manages the blood glucose content in your body. Overeating sugar may trigger insulin resistance, linked to a higher risk of diabetes, heart problems, and brain diseases.
Can natural sugar cause diabetes?
Foods you eat can cause diabetes, especially type 2 diabetes (1).
The major problem with type 2 diabetes is eating excessive amounts of added sugar and unhealthy carbs. This unhealthy habit can make you gain weight and have trouble with insulin (4, 9). A study showed that consuming a serving of sugary drinks daily may increase your risk of type 2 diabetes by 13% (22).
However, it’s not true for natural sugar.
Natural sugar and diabetes
Natural sugars found in fruits and vegetables, with no extra sugar added during manufacturing or processing, won’t make you more likely to get type 2 diabetes (18).
The glycemic index (GI) measures how fast food can cause blood sugar spikes. Low GI means slow sugar rise. Most fruits and vegetables have low to moderate GI values (23, 24).
These natural sugars are absorbed slowly due to the fiber, water, antioxidants, and other nutrient content (25, 26, 27). Also, eating more fiber-loaded fruit, like blueberries, may reduce your risk of type 2 diabetes (28, 29).
Large-scale studies show that the risk of type 2 diabetes decreased by 7‒12% and 10% for each additional daily serving of fruit and green leafy vegetables, respectively (30, 31, 32, 33).
Each 100 grams of fruit can contain up to 90 grams of sugar, but most fruits provide less than 20 grams (2). You don’t have to cut out fruits completely, be sugar-savvy, and practice portion control.
Fruit juice – Is it bad for people with diabetes?
Fresh fruits, like zesty citrus or berries, are a healthy vitamin boost for diabetes (34). Yet juicing strips off the fiber (27). Fruit juice has a higher GI than whole fruits (24, 36).
One cup of store-bought fruit juice contains 30 grams of carbs (35), a sugar rush for your blood (26, 30).
Studies also found that drinking a lot of fruit juice with added sugar increased the risk of developing type 2 diabetes by 28% than infrequent drinking. However, drinking 100% fruit juice with no added sugar didn’t increase the risk (37).
If you crave fruit juice, try to make it yourself and keep it in moderation.
Effects of artificial sweeteners on diabetes: Things you should know
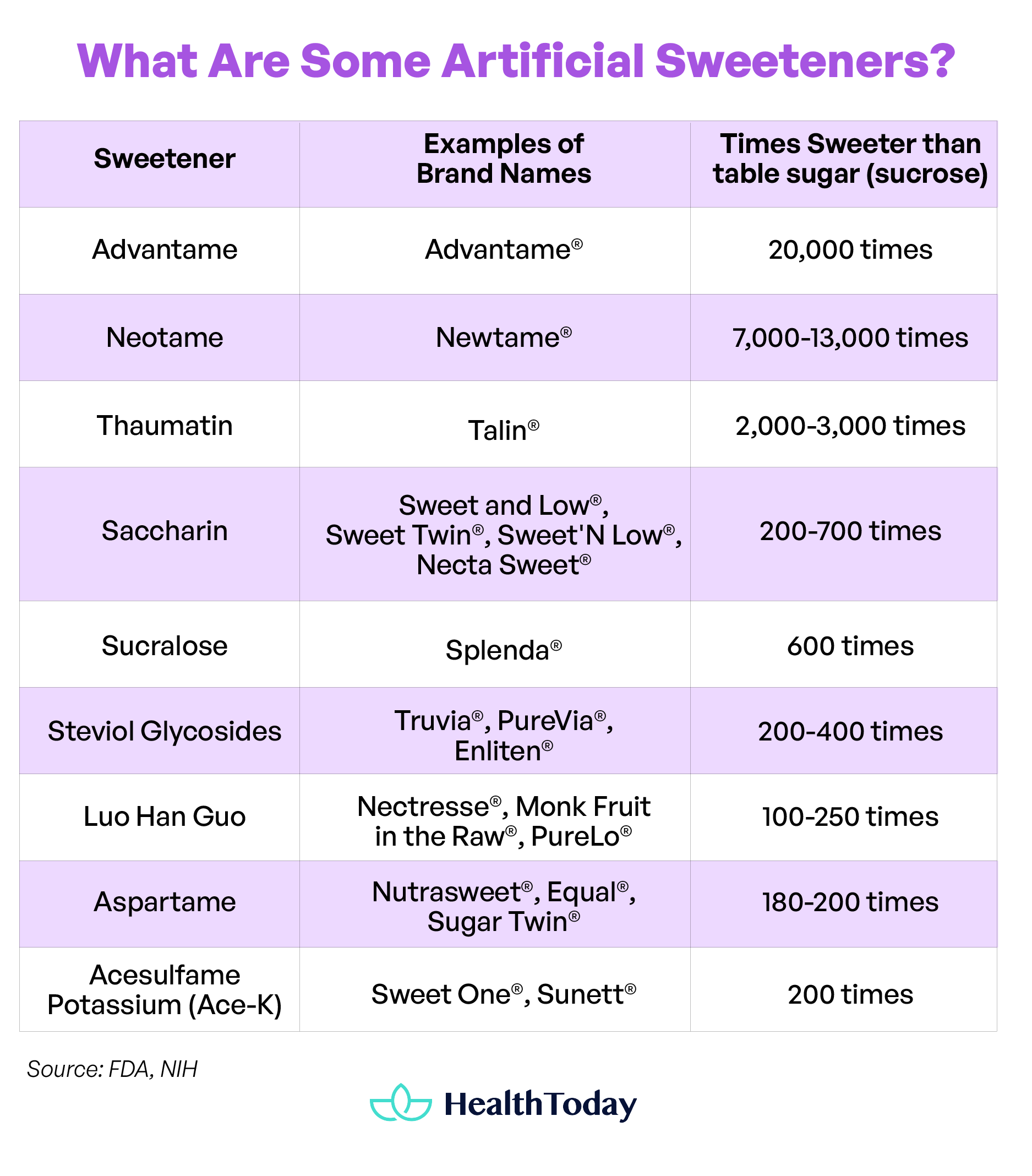
Aspartame, sucralose, and stevia are the sugar substitutes in many ‘diet’ or ‘sugar-free’ treats (38).
Artificial sweeteners are 200—20,000 times sweeter than table sugar (sucrose). The US Food and Drug Administration (FDA) approved some of them, including saccharin, aspartame, acesulfame potassium (Ace-K), neotame, and advantame. There are also sweeteners from plants and fruit, like Stevia, Luo Han Guo, and thaumatin (38, 39).
The question is: Do these sweeteners keep your blood sugar stable?
Although these sweeteners are calorie- or sugar-free, it’s uncertain about their effects on a regular use basis (40). People with phenylketonuria (PKU), a rare genetic disorder, should avoid or limit aspartame. It is hard for their bodies to process this (39).
Many studies revealed that ‘diet’ or ‘light’ foods and drinks might lead to weight gain, not weight loss (41), which can be due to their ability to disrupt our gut microbiota’s balance and diversity. It can contribute to obesity, insulin resistance, and classic diabetes risk factors (40, 42).
Artificial sweeteners can worsen glucose clearance (blood sugar removal). Studies in mice showed that consuming saccharin, sucralose, and aspartame for one week resulted in glucose intolerance and affected the gut microbiota composition. In healthy people, saccharin can provoke these effects (26, 40).
Consuming artificially sweetened products may also increase cravings, sugar intake, weight gain, and increasing the risk of diabetes (43).
Studies show a 38‒68% increased risk of diabetes from diet soda (44), which contains artificial sweeteners and acids(45, 46). However, acid is not known as a diabetes risk factor.
Having diet sodas or other ‘diet’ drinks is linked to heart and metabolism issues (40, 44):
- big waist
- brain-related diseases
- depression
- kidney function decline
- high blood pressure
- stroke and heart attack
- cancer
Artificially sweetened foods and drinks provide almost no added sugar and calories. However, they are still tied to the risk of developing diabetes. This can be attributable to their effects on gut microbiota and hunger cues.
Ate too much sugar? What you should do to detox
Currently, 63% of Americans exceed their recommended daily calories from added sugars. Adult men and women consume 19 and 15 teaspoons of added sugars per day on average, respectively (47, 48).
Are you going on sweet overload?
It’s no surprise: Eating too much sugar can directly spike your blood sugar. Some signs of high blood sugar are (49):
- Feeling very thirsty or having a dry mouth
- Having dry skin
- Feeling weak or tired
- Needing to pee often
- Experiencing blurry vision
Be mindful of sugar intake
Note that dietary sugar is vital for your body to function (3), but you should skip the added sugars and use natural, nutrient-dense options like fruits and milk (19).
Watch out for that sugar count. It can get tricky with the sneaky names for added sugars (418, 50, 51):
- Ingredient names ending in ‘ose’: sucrose (table sugar), fructose, lactose, glucose, maltose, and dextrose
- Natural sweeteners are still considered added sugar. They are honey, fruit juice concentrates, fruit nectars (such as agave nectar), coconut sugar, and cane juice, cane sugar.
- Invert sugar, cane crystals, brown sugar, corn syrup, malt syrup, maple syrup, and molasses are also added sugars.
Sugary drinks, such as soda, fruit drinks, and sports or energy drinks, account for 35% of the drinks consumed in the US. Desserts and sweet snacks account for 19%. They include candies, cookies, cakes, ice cream, frozen yogurt, doughnuts, sweet rolls, and pastries (48, 52).
Break the habit
If you want sugar detox, reduce carb intake and eat more soluble fiber. Over time, sweet cravings may decrease, and certain foods may even begin to taste overly sugary (18).
Here is a simple guide for you (18, 35, 53):
- For breakfast, keep carbs to less than half your calories and eat at least 2 grams of fiber.
- Juice time? Grab the 100% pure ones, and keep those portions steady.
- When baking, swap out half of your sugar with unsweetened applesauce or some mashed-up ripe banana.
- Are those sweet cravings knocking? Go for a 1/4 cup of unsweetened dried fruit, a full cup of juicy ripe fruit, or a 1-ounce square of 75% dark chocolate.
- If you are longing for high-sugar treats, scale down your portion. Savor it slowly, and make every bite a moment.
- Dinner on the radar: go for smaller carb servings, especially if it’s late at night. When you’re shopping, read the label. If the added sugars are 5% or less, it’s in the low zone. But hitting 20% or more is a high alert (18).
Be careful to check the serving size for drinks that come in large bottles. The amount in “one serving” may vary depending on the manufacturer. For some drinks, a “serving” means a whole 20-ounce bottle, while some may mean a standard 8 ounces (18).
Watch out for those ready-to-eat cereals, cereal bars, and quick-and-easy flavored oatmeals or pastries because they might hide more added sugars than expected (18, 54). Companies might advertise that their cereals contain whole grains, fiber, and vitamins, but all those nutrients can be easily found in fruits and veggies (19, 54).
Best sugar alternatives for people with diabetes:
If you crave that sweetness, eat fruits (25). The juicy deal is that they contain more fiber for extra fullness and blood sugar control (27, 29).
Whole-grain toast with nut butter or a bowl of oatmeal can be a healthy option to start your day. Sprinkle in sliced ripe bananas or toss in berries for an extra delight (18).
Check out these great alternatives for sugar-loaded drinks (18, 20, 35, 48):
- Plain water: Classic but always wins the game, whether tap, bottled, or bubbly. Spice it up with a hint of citrus fruits, berries, peaches, or a cucumber, along with some fresh herbs.
- Milk: Opt for lean—low-fat, or non-fat (skim) milk. Or, try those fortified with soy, rice, or almond, but do a sugar check first. They’re a vitamin and mineral boost.
- Yogurt: If you miss that creaminess. Elevate the experience with a scoop of fresh or frozen fruit and a dash of cinnamon.
- Tea and coffee: For a wake-me-up, try unsweetened tea or black coffee. Both are very low in calories and carbs. Don’t worry about the mild dehydration effect of caffeine. It won’t significantly affect your total daily fluid intake (55).
100% juice (whether it’s from veggies or fruits) and kombucha (50).
Does candy cause diabetes?
What actually causes diabetes?
Doctors do not fully know why people get type 1 diabetes. They suggest that genes and viruses set off the body’s defense (immune) system (8).
Type 2 diabetes and gestational diabetes are caused by insulin resistance. Other risk factors include sedentary behavior, poor diet, obesity, genetics, aging, and ethnicity (9, 16).
Is diabetes caused by fat or sugar?
One factor can’t cause diabetes. Type 1 diabetes is a disease where the body’s immune system attacks itself. Genes and viruses might be part of the puzzle (8). There is no solid proof that eating too much sugar or fat causes type 1 diabetes.
Type 2 diabetes means your body has trouble using insulin. Overconsumption of unhealthy fat and added sugar or being overweight may increase the risk (4, 9).
What is the main food enemy of diabetes?
Eating too much sugar can make it harder for the body to use insulin, which is a tough puzzle for diabetes. So, sugary treats and high-glycemic foods (like white rice or bread) should be avoided (4, 24). Also, stay away from processed foods high in trans fats. as they can contribute to insulin resistance (57).
Can alcohol cause diabetes?
Drinking alcohol doesn’t directly cause diabetes but can increase type 2 diabetes risk and impact diabetes management. If you drink a lot over time and you don’t eat enough, your blood sugar might take a dive, which is dangerous (58, 59).
Drinking alcohol can also make diabetes problems worse, like impaired liver function, nerve damage, and eye disease (4, 59).
Summary
Your body doesn’t need carbohydrates from added sugars to function properly.
So, can you get diabetes from eating sugar? Sugar does not directly cause diabetes, but increased sugar intake is associated with a higher risk of developing type 2 diabetes. Natural sugar from fruits and vegetables can be good alternatives.
Also, there is no answer to:” How much sugar causes diabetes?”. Yet, it is recommended to consume less than 10% of your daily calorie intake from added sugar.
Check the ingredients list, and skip foods that list sugar as the first or second ingredient. Make sure you scan the full list of ingredients, as some products may use different sweeteners.

















Comments
0